Antihistamines and Dementia Risk: What You Need to Know About Long-Term Use
 Jan, 19 2026
Jan, 19 2026
Anticholinergic Burden Calculator
How This Tool Works
The Anticholinergic Cognitive Burden (ACB) Scale rates medications from 0 to 3 based on brain impact. This tool calculates your total ACB score from multiple medications. A score of 3 or higher indicates potential dementia risk according to medical guidelines.
Enter your medications below. Each medication's ACB score is based on the article's reference:
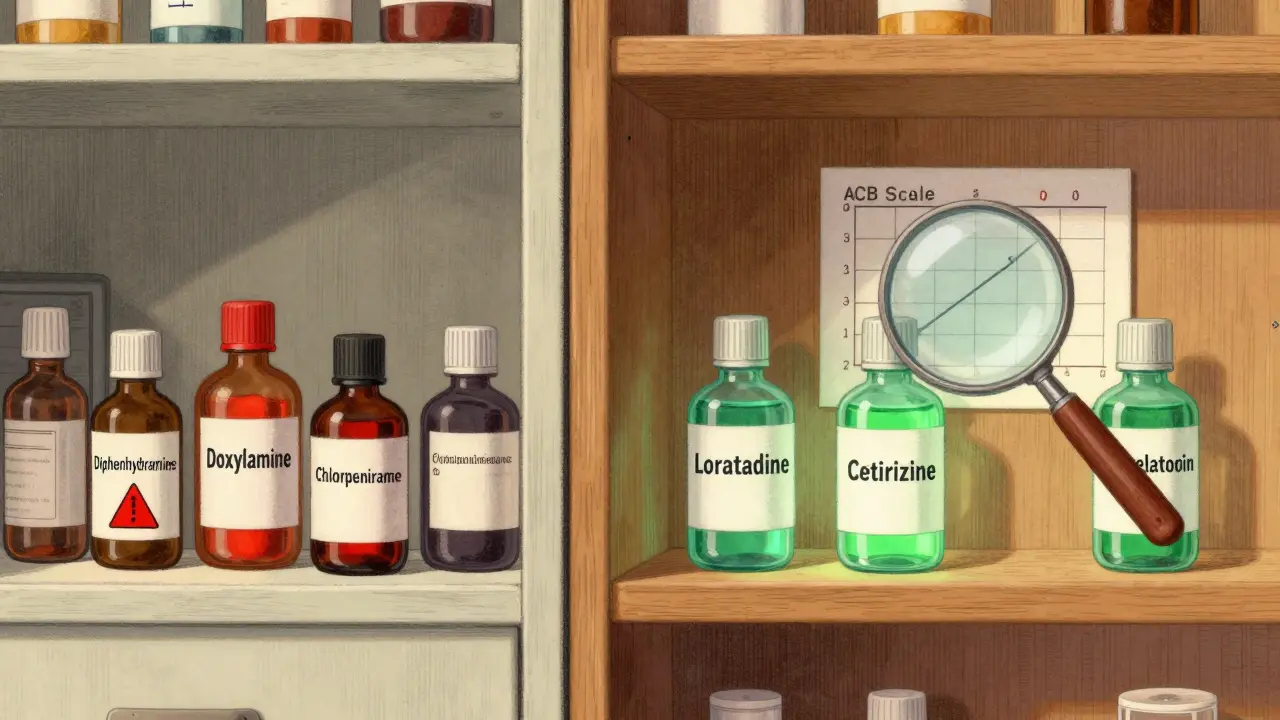
- Score 0: Second-gen antihistamines (loratadine, cetirizine, fexofenadine)
- Score 1: Low anticholinergic drugs (e.g., doxepin)
- Score 2: Moderate anticholinergic drugs
- Score 3: High anticholinergic drugs (e.g., diphenhydramine)
Your Anticholinergic Burden
For decades, diphenhydramine - the active ingredient in Benadryl - has been a go-to sleep aid for older adults. Easy to find, cheap, and fast-acting, it seemed harmless. But now, doctors are warning that nightly use might be doing more harm than good. The concern isn’t just drowsiness the next day. It’s something deeper: a possible link to dementia.
Why Some Antihistamines Are Riskier Than Others
Not all antihistamines are the same. There are two main types: first-generation and second-generation. The first-generation ones - like diphenhydramine, doxylamine, and chlorpheniramine - cross the blood-brain barrier. Once inside, they block acetylcholine, a brain chemical critical for memory and thinking. This is called anticholinergic activity. It’s why these drugs make you sleepy, but it’s also why they might hurt your brain over time.Second-generation antihistamines - like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) - were designed differently. They don’t cross into the brain as easily. That’s why they don’t cause drowsiness in most people. And crucially, they have almost no anticholinergic effect. If you’re taking an antihistamine regularly, switching to one of these is one of the safest changes you can make.
What the Research Actually Shows
A 2015 study from JAMA Internal Medicine got a lot of attention. It followed over 3,400 people aged 65 and older for 10 years. Those who took strong anticholinergic drugs - including first-gen antihistamines - for three years or more had a higher risk of dementia. But here’s what many people miss: when researchers looked at antihistamines alone, the risk didn’t hold up.A follow-up study in 2019 found that antidepressants, bladder meds, and Parkinson’s drugs showed clear links to dementia. Antihistamines? No significant increase. Another 2022 study of nearly 9,000 seniors found dementia rates of 3.8% in first-gen users versus 1% in second-gen users - but after adjusting for other factors, the difference wasn’t statistically meaningful.
So why do doctors still warn against first-gen antihistamines? Because the evidence isn’t clean. Some studies show risk. Others don’t. The American Geriatrics Society, which sets guidelines for older adults, says to avoid them anyway. Why? Because the potential harm is real, and the benefit is weak. If you’re taking diphenhydramine for sleep, you’re trading short-term drowsiness for a possible long-term cost - and there are better options.
The Anticholinergic Burden Scale: A Simple Tool
Doctors use a tool called the Anticholinergic Cognitive Burden (ACB) Scale to rate how much a drug affects the brain. Diphenhydramine scores a 3 - the highest possible. That means it’s strongly anticholinergic. Fexofenadine? Score of 0. No effect. Loratadine? Also 0.Here’s the thing: it’s not just antihistamines. Many common medications add up. A painkiller, a bladder pill, a sleep aid - each with a small anticholinergic score - can stack up to a dangerous total. That’s why experts recommend reviewing all your meds every six months. Ask your doctor: “What’s the ACB score for each of these?” If you’re taking three or more drugs with a score of 1 or higher, you’re in the risk zone.
What About Over-the-Counter Sleep Aids?
About 42% of adults over 65 use OTC sleep aids. Most of them contain diphenhydramine. And 78% of those users have no idea it’s an anticholinergic. That’s a huge gap.On Reddit, a geriatric care manager shared that 83% of her clients over 70 take Benadryl nightly. One woman on AgingCare.com wrote: “My mother’s doctor prescribed Benadryl for years to help her sleep, and now she has dementia - I can’t help but wonder.” She’s not alone. People connect the dots. And while science hasn’t proven a direct cause, the pattern is too common to ignore.
Even the FDA hasn’t required dementia warnings on OTC labels - only “may cause drowsiness.” Meanwhile, the European Medicines Agency updated labels in 2022 to include “potential long-term cognitive effects with prolonged use.” The U.S. is lagging.
Real Alternatives That Actually Work
You don’t have to suffer through insomnia. There are safer, proven options.- Cognitive Behavioral Therapy for Insomnia (CBT-I): This isn’t just talk therapy. It’s a structured program that teaches you how to sleep better without drugs. Studies show it works for 70-80% of older adults. The catch? Finding a therapist. Wait times average over two months, and Medicare only pays $85-$120 per session.
- Low-dose doxepin (Silenor): This prescription sleep aid has minimal anticholinergic effects (ACB score of 1). It’s been used since 2010 and now makes up 12% of the prescription sleep market.
- Melatonin: Especially for circadian rhythm issues. A 0.3-1 mg dose taken 30 minutes before bed helps many seniors fall asleep faster - without brain effects.
- Good sleep hygiene: No screens after 8 p.m., consistent bedtime, cool room, no caffeine after noon. Simple, but powerful.
One woman in her late 70s switched from Benadryl to melatonin and CBT-I. Within six weeks, she was sleeping better and felt more alert during the day. She didn’t need a pill anymore.

What’s Changing in 2024 and Beyond
New research is underway. The ABCO study, funded by the NIH, is tracking 5,000 older adults for 10 years with detailed medication logs and yearly brain tests. Early data from the UK Biobank suggests that when you account for underlying sleep disorders, antihistamine use itself doesn’t raise dementia risk. That’s a big deal - it means the problem might not be the drug, but the reason people take it.The American Geriatrics Society is updating its Beers Criteria in June 2024. Expect clearer, drug-specific warnings. Meanwhile, the FDA is reviewing all anticholinergic medications. A decision is expected by mid-2024.
Market trends are already shifting. First-gen antihistamine sales dropped 24% between 2015 and 2022. Second-gen sales jumped 18%. More people are asking for safer options. Pharmacies are starting to stock more non-anticholinergic sleep aids. The tide is turning.
What You Should Do Right Now
If you or someone you love is taking diphenhydramine, doxylamine, or chlorpheniramine regularly - even just a few times a week - here’s what to do:- Check the label. Look for “diphenhydramine,” “doxylamine,” or “anticholinergic” on the drug facts panel.
- Ask your doctor or pharmacist. Say: “Is this drug anticholinergic? Is there a safer alternative?”
- Switch to a second-gen antihistamine. If it’s for allergies, go with loratadine or cetirizine. If it’s for sleep, try melatonin or talk about CBT-I.
- Review all meds. Get a full list of everything you take. Add up the ACB scores. If it’s 3 or higher, talk to your doctor about cutting back.
- Don’t quit cold turkey. Stopping diphenhydramine suddenly can cause rebound insomnia. Taper slowly under medical supervision.
There’s no need to panic. But there’s every reason to act. The science isn’t settled. But the advice from experts is clear: avoid first-gen antihistamines in older adults. The risks are real. The alternatives exist. And your brain deserves better than a pill that makes you sleepy tonight - and might hurt you tomorrow.

Samuel Mendoza
January 20, 2026 AT 01:44Stop panicking. The study they cited had a 3.8% vs 1% rate - that’s not a crisis, it’s noise. People who take Benadryl nightly are already the ones with poor sleep hygiene, chronic pain, or depression - all of which raise dementia risk. Correlation isn’t causation, and you’re selling fear to sell supplements.
Glenda Marínez Granados
January 20, 2026 AT 21:26So let me get this straight… we’re supposed to trust a medical establishment that told us smoking was ‘good for the nerves’ and that estrogen was a fountain of youth… and now they’re telling us Benadryl is the devil? 😏
Next they’ll ban aspirin because ‘it might cause existential dread.’
Yuri Hyuga
January 21, 2026 AT 16:43Let’s reframe this: it’s not about fear - it’s about empowerment. 🌱
If you’re taking diphenhydramine for sleep, you’re not ‘just using an OTC aid’ - you’re using a band-aid on a broken system. The real win? Finding CBT-I. It’s not glamorous, but it’s life-changing. I’ve seen 70-year-olds reclaim their nights - no pills, no guilt, just better sleep. You deserve that peace. Start small. Talk to your pharmacist today. You’ve got this.
MARILYN ONEILL
January 21, 2026 AT 20:33I read the whole thing and honestly? This is just another way for doctors to make money. Melatonin? That’s a supplement. CBT-I? That’s expensive. Benadryl is $5 and works. If you’re old enough to need sleep, you’re old enough to deal with a little drowsiness. Stop overcomplicating everything.
Coral Bosley
January 22, 2026 AT 14:30My grandma took Benadryl for 15 years. She never had dementia. She had arthritis, depression, and a dog that barked at 3 a.m. She wasn’t taking it because she was stupid - she was taking it because she was tired. Now they want her to sit in a room for 8 weeks talking about her ‘sleep hygiene’? Give me a break. This isn’t prevention - it’s condescension wrapped in jargon.
Steve Hesketh
January 24, 2026 AT 10:01Brothers and sisters - I want you to pause for a second. 🤲
There are millions of people - especially in communities without access to specialists - who rely on these pills because they have no other choice. We can’t shame them. We can’t just say ‘switch to melatonin’ when your local pharmacy doesn’t carry it and your doctor won’t return your call. Let’s fix the system - not the person. We need more clinics, more education, more compassion. This isn’t about blame - it’s about care.
MAHENDRA MEGHWAL
January 25, 2026 AT 00:21It is imperative to acknowledge that the pharmacological profiles of first-generation antihistamines demonstrate a demonstrable affinity for muscarinic receptors, thereby inducing a state of cholinergic suppression. The longitudinal data, while not universally conclusive, present a statistically significant trend in cognitive decline among chronic users, particularly when polypharmacy is present. Therefore, it is prudent to exercise caution and prioritize agents with negligible anticholinergic burden, such as loratadine, in geriatric pharmacotherapy.
Dee Monroe
January 25, 2026 AT 11:26I’ve been thinking about this a lot. It’s not just about the drug - it’s about what we’ve allowed our society to become. We’ve turned sleep into a problem to be solved with a pill, not a rhythm to be restored. We’ve normalized exhaustion. We’ve made ‘I’m so tired’ a badge of honor. And then we’re shocked when our brains start to fog? We don’t need more warnings on labels - we need to stop glorifying burnout. Maybe the real anticholinergic isn’t diphenhydramine… it’s our culture.
Kelly McRainey Moore
January 26, 2026 AT 16:53My mom switched from Benadryl to melatonin last year. She says she sleeps better and doesn’t feel like a zombie in the morning. No drama. Just… better. I’m glad she listened to her pharmacist.
michelle Brownsea
January 27, 2026 AT 06:43Let me be perfectly clear: if you are taking a first-generation antihistamine regularly - and you are over the age of 60 - you are not ‘just being cautious’; you are actively exposing your hippocampus to neurotoxic stressors. The ACB scale is not a suggestion - it is a clinical imperative. Ignoring it is not ‘natural living’ - it is negligence. And if you think melatonin is ‘just a supplement,’ you clearly haven’t read the FDA’s adverse event reports from 2021. Wake up.
Malvina Tomja
January 27, 2026 AT 18:44Everyone’s acting like this is some big revelation. Newsflash: Benadryl makes you drowsy. Drowsiness = brain fog. Brain fog over time = memory issues. Duh. The fact that people are shocked by this proves how little they know about how their own bodies work. Also - if you’re still using ZzzQuil, you’re not ‘old,’ you’re just lazy.
Melanie Pearson
January 28, 2026 AT 22:51This article is dangerous. It’s pushing a globalist medical agenda. In America, we have the right to choose what we put in our bodies. The FDA doesn’t warn you - because they’re asleep at the wheel. But Europe? They’re always overreacting. Don’t let them tell you what to take. Benadryl has saved my nights for 20 years. I’m not switching to some ‘melatonin trend’ just because some PhD in London says so.
Uju Megafu
January 30, 2026 AT 15:39Y’all are acting like this is the first time someone’s been told ‘your meds might be killing you.’ Remember when they said Tylenol was fine for babies? Then it wasn’t. Remember when they said trans fats were safe? Then they weren’t. Now it’s Benadryl. Tomorrow? It’ll be ibuprofen. They’ll make you pay for every breath. They don’t care about you - they care about profit. Wake up. Don’t be the next victim.
Jarrod Flesch
February 1, 2026 AT 10:39Just want to say - if you’re reading this and you’re scared, you’re not alone. I helped my dad switch from Benadryl to low-dose doxepin last year. Took 6 weeks. He cried the first night he slept without a pill. But now? He’s laughing again. He remembers names. He plays chess. It’s not magic - it’s just better choices. You can do this. 💪