Citalopram and Escitalopram: QT Prolongation Risks and Safe Dose Limits
 Dec, 4 2025
Dec, 4 2025
QT Prolongation Risk Calculator
When you’re prescribed an antidepressant, you’re usually focused on how it will help your mood, sleep, or anxiety. But there’s one quiet risk that doesn’t get talked about enough: QT prolongation. Two of the most common SSRIs - citalopram and escitalopram - carry this risk, and the dose you take can make a big difference. If you’re over 65, have heart issues, or take other meds, this isn’t just a footnote. It’s something you need to know.
What’s QT Prolongation, and Why Should You Care?
Your heart beats because of electrical signals. The QT interval on an ECG measures how long it takes for your heart’s lower chambers to recharge between beats. If that interval gets too long, your heart can develop dangerous rhythms - like Torsade de Pointes - which can lead to fainting, seizures, or even sudden death.
Citalopram and escitalopram both block a specific potassium channel in the heart called hERG. That’s how they help with depression - by increasing serotonin in the brain. But that same action slows down the heart’s recharge time. It’s a side effect built into the chemistry.
It’s not common. Most people take these meds without any heart issues. But when the risk spikes - usually at higher doses or in vulnerable people - it becomes serious enough for global health agencies to step in.
The 2011 Safety Wake-Up Call
In August 2011, the U.S. FDA issued a clear warning: high doses of citalopram could cause dangerous heart rhythm changes. By December, the UK’s MHRA followed suit - but this time, they included escitalopram too. New Zealand’s Medsafe added their warning in March 2012. This wasn’t a rumor. It was based on clinical studies showing clear, dose-dependent QT prolongation.
Here’s what the data showed:
- Citalopram at 20mg: +8.5ms QTc increase
- Citalopram at 40mg: +12.6ms QTc increase
- Citalopram at 60mg: +18.5ms QTc increase
- Escitalopram at 10mg: +4.5ms QTc increase
- Escitalopram at 20mg: +6.6ms QTc increase
- Escitalopram at 30mg: +10.7ms QTc increase
These numbers aren’t just lab results. They’re real changes seen in people’s ECGs. And while a 10-20ms shift might sound small, the threshold for concern is 500ms absolute QTc - or a rise of 60ms from your baseline. That’s when the risk of dangerous arrhythmias jumps.
Dose Limits: What’s Safe Now?
After the 2011 warnings, dose limits were set - and they’re not suggestions. They’re hard caps for safety.
Citalopram:
- Under 65: Max 40mg per day
- Over 65 or with liver problems: Max 20mg per day
Escitalopram:
- Under 65: Max 20mg per day
- Over 65 or with liver problems: Max 10mg per day
These limits are based on how your body processes the drug. Older adults and people with liver impairment clear these medications slower. That means more drug in your system - and a higher chance of QT prolongation.
Even at approved doses, you shouldn’t just start high. Doctors are supposed to begin low - 10mg for citalopram, 5-10mg for escitalopram - and increase slowly only if needed. If you’re feeling worse after a dose increase, or if you’ve had dizziness, palpitations, or fainting, get an ECG. Don’t wait.
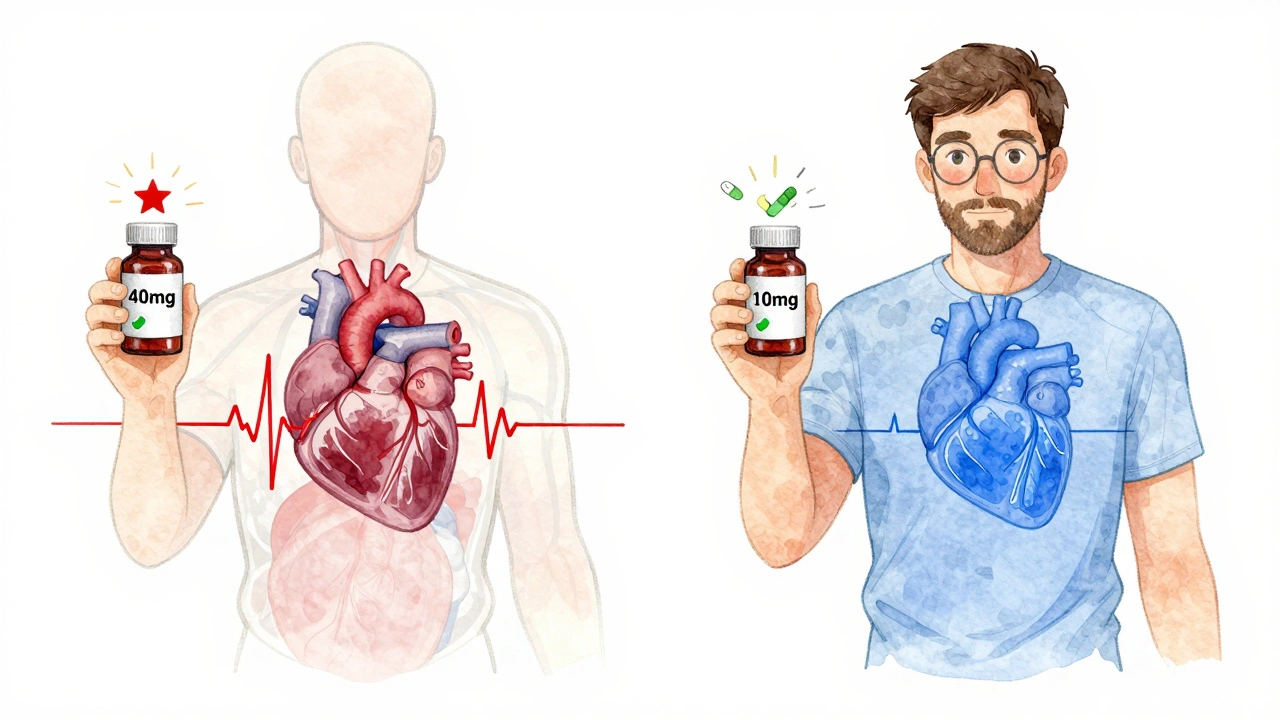
Citalopram vs. Escitalopram: Which Is Safer?
Escitalopram is the purified form of citalopram. Citalopram is a mix of two mirror-image molecules (enantiomers); only one of them (the S-form) works for depression. The other (R-form) doesn’t help with mood - but it does contribute to QT prolongation.
That’s why escitalopram generally causes less QT prolongation at equivalent doses. At 20mg, escitalopram adds about 6.6ms to your QTc. Citalopram at the same dose? About 12.6ms. That’s nearly double.
But here’s the catch: some studies say the actual risk of Torsade de Pointes is similar between the two. Why? Because even though citalopram causes bigger QT changes, escitalopram is often prescribed at higher doses than it should be - and people still take it with other heart-affecting drugs.
So while escitalopram has a better safety profile on paper, the real-world risk depends on how it’s used. For someone with heart disease, diabetes, or a history of arrhythmia, escitalopram at 10mg is often the safer pick. For someone with no cardiac history and no other meds, citalopram at 20mg might still be fine - but only if monitored.
Who’s at Highest Risk?
It’s not just about the dose. Other factors stack the deck:
- Age over 65
- History of heart disease, heart failure, or prior QT prolongation
- Low potassium or magnesium levels
- Slow heart rate (bradycardia)
- Family history of sudden cardiac death or long QT syndrome
- Taking other QT-prolonging drugs - like certain antibiotics (macrolides, fluoroquinolones), antifungals, antiarrhythmics, or even some antipsychotics
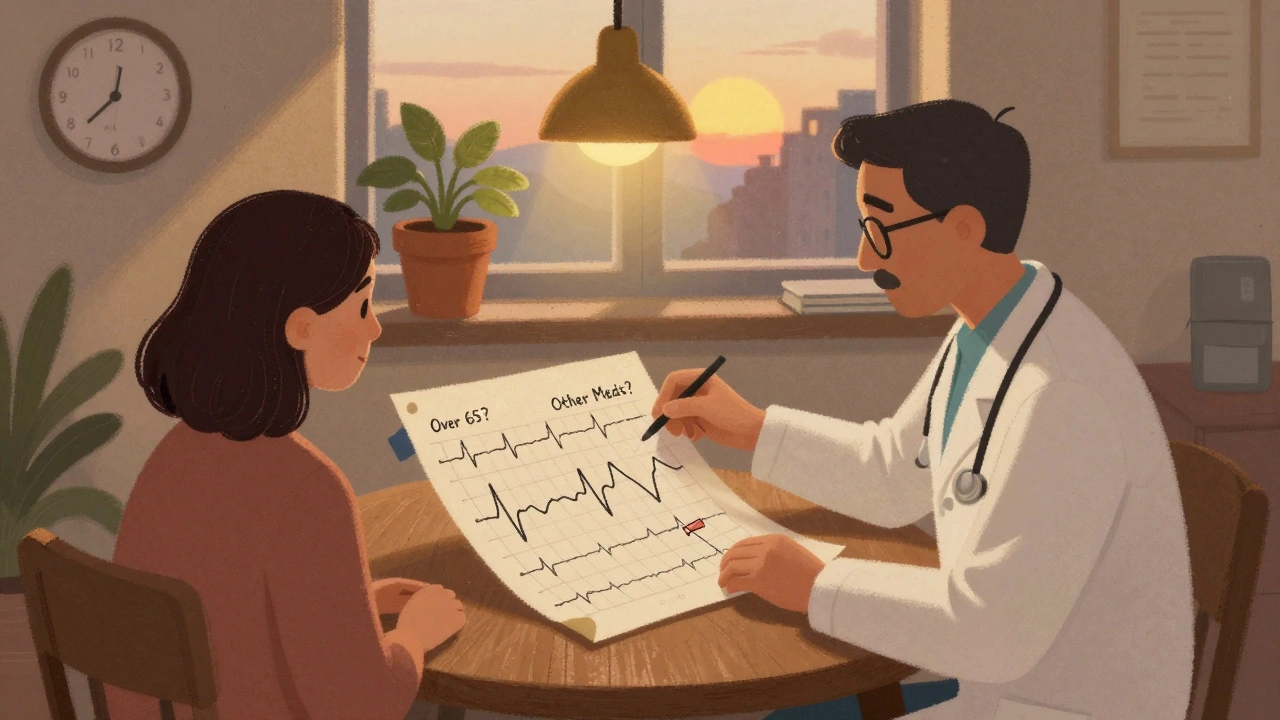
If you’re on any of these, your doctor should check your ECG before starting either medication - and again after 1-2 weeks if the dose is increased.
And don’t assume your pharmacist knows. Many don’t automatically flag drug interactions unless you ask. If you’re on citalopram or escitalopram and get a new prescription - even for a cold or infection - ask: “Could this affect my heart rhythm?”
Other Antidepressants: What’s Safer?
If you’re worried about QT risk, you have alternatives:
- Fluoxetine: Minimal QT effect. Often used long-term.
- Sertraline: Very low risk at standard doses.
- Paroxetine: Also low risk.
- Fluvoxamine: Safe for cardiac patients.
- Mirtazapine: Not an SSRI, but no QT prolongation.
Tricyclics like amitriptyline and maprotiline can prolong QT too - sometimes even more than citalopram. So switching to an older antidepressant isn’t always safer.
Venlafaxine (an SNRI) is generally low risk - unless you overdose. Then it becomes dangerous.
For most people, fluoxetine or sertraline are better first choices if cardiac risk is a concern. But if you’ve tried those and they didn’t work, escitalopram at 10mg is still a valid option - just with more monitoring.
What Should You Do?
Here’s what to do if you’re on citalopram or escitalopram:
- Know your dose. Don’t take more than the limit - even if you feel like you need more.
- Ask for an ECG if you’re over 65, have heart issues, or are on other meds.
- Get blood tests for potassium and magnesium if you’re on diuretics or have poor diet.
- Report dizziness, fainting, rapid heartbeat, or palpitations immediately.
- Don’t stop cold turkey. Depression can worsen. Talk to your doctor about tapering if needed.
These meds work. Millions take them safely every day. But safety isn’t about avoiding risk entirely - it’s about managing it. If you’re on the right dose, with the right monitoring, the benefits still outweigh the risks.
Bottom Line
Citalopram and escitalopram are effective antidepressants - but they’re not risk-free. The QT prolongation danger is real, dose-dependent, and well-documented. The good news? The limits are clear. The warnings are out. And for most people, sticking to the recommended doses makes these drugs safe to use.
If you’re unsure, ask your doctor: “Is my dose safe for my heart?” That one question could prevent a serious problem. Don’t assume it’s fine because you feel better. Your heart doesn’t always give you symptoms before it’s too late.
Can I take citalopram or escitalopram if I have a pacemaker?
Yes, but with caution. A pacemaker can help prevent dangerous slow heart rhythms, but it doesn’t stop Torsade de Pointes. Both drugs can still prolong the QT interval, and pacemakers don’t correct that. Your doctor should monitor your ECG and may prefer escitalopram at the lowest effective dose. Always tell your cardiologist you’re taking either medication.
Is escitalopram always safer than citalopram?
Generally, yes - because it causes less QT prolongation at equivalent doses. But if you’re taking escitalopram at 20mg, you’re getting nearly the same cardiac risk as citalopram at 40mg. The key is staying within the recommended limits. Escitalopram isn’t a free pass to take higher doses.
How often should I get an ECG if I’m on these meds?
If you’re over 65, have heart disease, or are on other QT-prolonging drugs, get an ECG before starting and again after 1-2 weeks if the dose is increased. For healthy adults under 65 on standard doses, routine ECGs aren’t usually needed unless symptoms appear. But if you’ve had a previous prolonged QT, your doctor may recommend yearly checks.
Can I drink alcohol while taking citalopram or escitalopram?
It’s best to avoid alcohol. Alcohol can lower potassium levels and slow liver metabolism, both of which increase QT prolongation risk. It also worsens dizziness and drowsiness - side effects already common with these drugs. Even one drink a day can add up, especially in older adults.
What if I accidentally took too much?
Call emergency services immediately. Overdose on either drug can cause severe QT prolongation, seizures, or cardiac arrest. Even if you feel fine, symptoms can appear hours later. Don’t wait. Bring the medication bottle with you to the hospital.
If you’re on citalopram or escitalopram, you’re not alone. But knowing the risks - and sticking to the limits - means you can keep taking them safely. Don’t let fear stop you. Just stay informed.

Katie Allan
December 5, 2025 AT 11:58Thank you for laying this out so clearly. I’ve been on escitalopram for years at 10mg and never realized how much the heart monitoring matters. I’m 68 and on a statin too-this post just made me schedule my ECG. You’re right: feeling better mentally doesn’t mean your heart is safe.
Ali Bradshaw
December 6, 2025 AT 07:32Been reading this while sipping tea. Honestly, this is the kind of info that should be printed on the prescription bottle. Not everyone has a cardiologist on speed dial. If your GP just hands you a script and says ‘take one daily,’ that’s not enough.
aditya dixit
December 7, 2025 AT 05:05As someone from India where cardiac screening is often overlooked, I’ve seen too many patients on SSRIs with no baseline ECG. This is vital. The dose limits aren’t arbitrary-they’re evidence-based. Doctors here often prescribe citalopram at 40mg without hesitation. This needs to be shared widely.
Juliet Morgan
December 7, 2025 AT 15:28i’ve been on 20mg of escitalopram for 3 years and never had an ekg. i feel fine. but now i’m scared. should i panic? or just call my dr tomorrow?
Mark Curry
December 9, 2025 AT 10:39Good post. I’m 72, on citalopram 20mg, and had a pacemaker put in last year. My cardiologist didn’t mention the QT risk-only that the pacemaker would handle slow heartbeats. Now I’m wondering if I need a repeat ECG. Thanks for the reminder.
Norene Fulwiler
December 10, 2025 AT 04:11This is exactly why I stopped prescribing citalopram to older patients. Escitalopram at 10mg is the new standard in my practice. But patients still ask why we can’t just go higher if they’re not feeling it. We can’t. The math doesn’t lie.
Chris Brown
December 11, 2025 AT 12:07Of course the FDA issued warnings. They’re always overreacting to pharmaceutical data. Back in the 90s, they said SSRIs caused suicide. Now it’s QT prolongation. Next it’ll be that breathing causes depression. The real issue is that people are medicated too easily.
an mo
December 13, 2025 AT 04:47Let’s be real: the pharmaceutical industry designed this. They knew citalopram’s R-enantiomer was cardiotoxic but marketed it anyway. Escitalopram was just a rebrand with a 300% price hike. The science is manipulated to sell more pills. Check the patent timelines.
William Chin
December 14, 2025 AT 06:40It is imperative that all individuals prescribed selective serotonin reuptake inhibitors undergo comprehensive cardiac risk stratification prior to initiation of therapy. The hERG channel blockade is a class effect, and the potential for torsades de pointes is non-trivial. Documentation of baseline QTc interval is mandatory.
Harry Nguyen
December 14, 2025 AT 09:57Wow. So the solution to mental health is… not taking medicine? Because apparently, if you’re over 65 or have a heartbeat, you’re just not allowed to feel better. Brilliant. Next they’ll ban coffee because it makes your heart race. Classic medical paternalism.
Lucy Kavanagh
December 14, 2025 AT 16:37Did you know the UK government secretly changed the dose limits because Big Pharma threatened to pull all antidepressants from the NHS? That’s why they lowered escitalopram to 10mg for seniors-it’s not safety, it’s cost-cutting. I’ve got a cousin in Brighton who got switched and now she’s crying all day. They don’t care.
Mark Ziegenbein
December 16, 2025 AT 13:57Let me be perfectly clear-the entire framework of SSRI prescribing is built on a foundation of statistical noise and industry-funded trials that ignore individual metabolic variance. The FDA limits are based on population averages, not physiology. Someone with CYP2C19 poor metabolizer status on 10mg of escitalopram could have plasma concentrations equivalent to 30mg in a fast metabolizer. Yet we treat everyone like a spreadsheet cell. This is not medicine. This is algorithmic tyranny.
Ada Maklagina
December 17, 2025 AT 02:17my dr gave me citalopram 40mg last year. i didn’t know it was too much. now i’m scared to tell them. what if they think i’m dumb?
Mellissa Landrum
December 18, 2025 AT 17:33lol i took 60mg of citalopram for 3 months because my dr said ‘it’s fine if you feel better’ and now i’m in a cardiac rehab program. the nurses said i’m lucky i didn’t drop dead. if you’re reading this and on high dose-stop. call your dr. don’t wait for your heart to say hi.