Clopidogrel and Proton Pump Inhibitors: What You Need to Know About Reduced Antiplatelet Effects
 Dec, 18 2025
Dec, 18 2025
Clopidogrel-PPI Interaction Checker
This tool helps you determine if the proton pump inhibitor (PPI) you're taking or considering is safe to use with clopidogrel. It shows the risk level based on scientific evidence about drug interactions.
Select your current PPI to see whether it could reduce clopidogrel's effectiveness and increase your risk of blood clots.
Interaction Information
Please select a PPI to see interaction details.
When you're on clopidogrel after a heart attack or stent placement, your body needs that drug to work properly. It stops platelets from clumping together and forming dangerous clots. But if you're also taking a proton pump inhibitor (PPI) for heartburn or stomach ulcers, something unexpected might be happening: clopidogrel could be losing its power.
Why This Interaction Matters
Clopidogrel doesn't work right away. Your liver has to convert it into an active form using an enzyme called CYP2C19. That’s the key. Some PPIs, especially omeprazole and esomeprazole, block that same enzyme. Think of it like two people trying to use the same narrow hallway at the same time. One person (clopidogrel) needs to get through to do their job. The other (omeprazole) stands in the way and slows them down.Studies show that when omeprazole is taken with clopidogrel, the amount of active clopidogrel in your blood can drop by nearly half. That’s not a small drop. It means your platelets might start sticking together again - exactly what you’re trying to prevent after a heart procedure.
Not All PPIs Are the Same
Here’s the good news: not every PPI causes this problem. The effect varies widely depending on the drug.- Omeprazole and esomeprazole: Strong CYP2C19 blockers. These are the ones linked to reduced clopidogrel effectiveness. Studies show platelet inhibition can drop below 20% - way below the therapeutic range.
- Lansoprazole: Mild effect. Some studies show a small reduction, but not enough to be clinically concerning in most cases.
- Pantoprazole and rabeprazole: Very weak or no effect. These are the safer choices when you need a PPI with clopidogrel.
A 2015 analysis in Circulation found that rabeprazole didn’t reduce clopidogrel’s active metabolite at all, while omeprazole cut it by 47%. That’s a huge difference. And it’s not just theory - real patients on omeprazole showed platelet activity levels that put them back at risk for clots.
What the Guidelines Say
Guidelines aren’t perfectly aligned, but they’re getting clearer.The American College of Cardiology and American Heart Association (2016) admit the interaction exists but say we don’t have solid proof it leads to more heart attacks or deaths. Meanwhile, the European Society of Cardiology and the UK’s NICE guidelines are more direct: avoid omeprazole and esomeprazole with clopidogrel. They say pantoprazole and rabeprazole are safe alternatives.
The FDA issued a warning in 2009 after early data showed increased cardiovascular events. The European Medicines Agency followed with similar restrictions. Today, most hospital pharmacies in the U.S. have switched their default PPI for clopidogrel patients from omeprazole to pantoprazole - a practice backed by a 2019 survey showing 72% of cardiologists prefer it.
Why Do Doctors Still Prescribe Omeprazole?
It’s cheaper. It’s widely available over the counter. Many patients already take it for reflux. But here’s the catch: if you’re on clopidogrel, that convenience might cost you.Despite warnings, a 2018 Medicare analysis found that omeprazole was still prescribed with clopidogrel in nearly 30% of cases. That number has dropped from 21% in 2010 to 8.7% in 2018 - progress, but not enough. Why? Because the evidence is messy. Some big trials, like COGENT, found no increase in heart events when omeprazole was added to clopidogrel. But those trials were designed for overall safety, not to measure platelet function.
Here’s the problem: platelet tests aren’t done in routine care. So if your clopidogrel isn’t working, you won’t know until something bad happens - a stent clot, a heart attack, a stroke.
Who Really Needs a PPI?
Not everyone on clopidogrel needs a PPI. But if you have risk factors for stomach bleeding, you absolutely should have one.These are the high-risk groups:
- Age 75 or older
- History of stomach or duodenal ulcers
- Taking NSAIDs like ibuprofen or naproxen
- Infected with H. pylori bacteria
For these people, PPIs cut the risk of GI bleeding by nearly 70%. That’s huge. The risk of a clot from weak clopidogrel? It’s real - but less common. So the decision isn’t just about drugs. It’s about balancing two dangers: bleeding versus clotting.
Does Timing Help?
Some patients ask: “What if I take my PPI in the morning and clopidogrel at night?”It doesn’t help. A study from the NIH showed that even when doses were separated by 12 hours, omeprazole still blocked clopidogrel’s effect. The enzyme inhibition lasts longer than the drug stays in your blood. So timing doesn’t fix this - switching PPIs does.
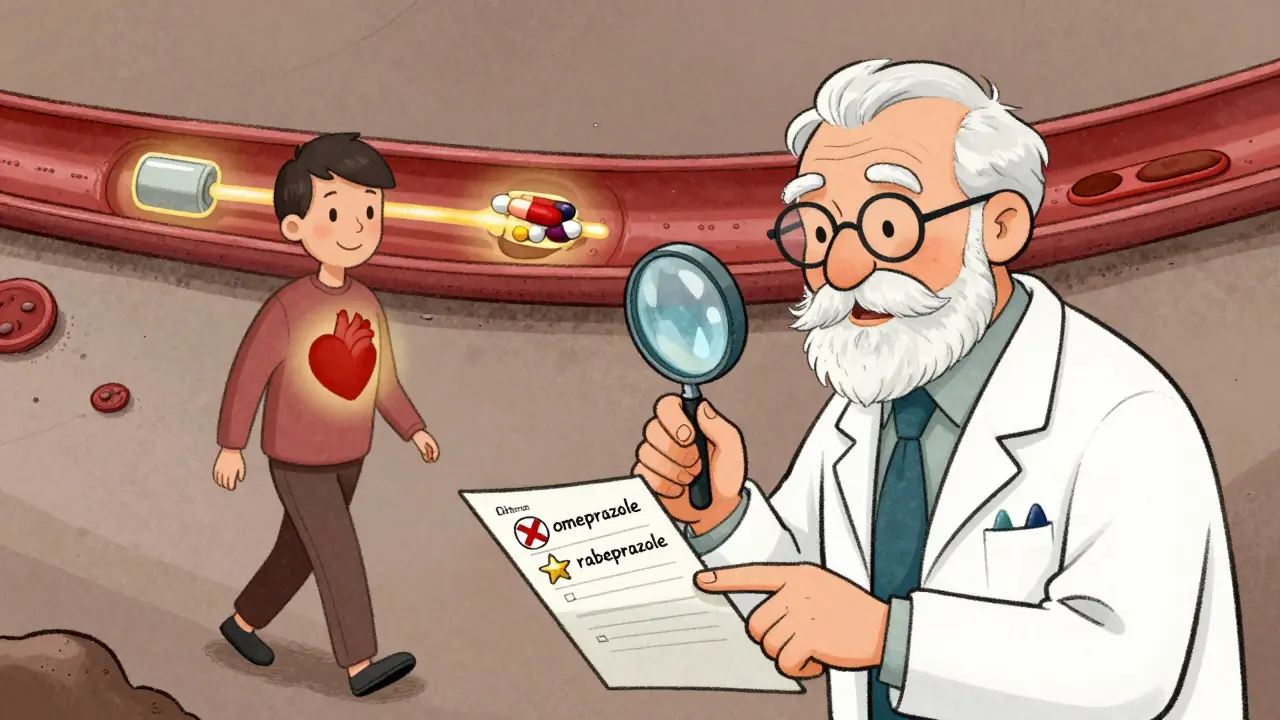
What Should You Do?
If you’re on clopidogrel and take a PPI:- Check which one you’re taking. Look at the label. Omeprazole? Esomeprazole? That’s a red flag.
- Ask your doctor or pharmacist if you can switch to pantoprazole or rabeprazole. Both are available as generics and cost about the same.
- If you’re unsure, get your platelet function tested. Some hospitals offer VASP or VerifyNow tests - they’re not routine, but they can clarify if clopidogrel is working.
- If you don’t need a PPI, consider stopping it. Not everyone does.
And if you’re starting clopidogrel now? Ask upfront: “What’s the safest PPI to use with this?” Don’t wait until you’re already on omeprazole.
The Bigger Picture: New Drugs Are Changing the Game
Clopidogrel isn’t the only option anymore. Newer antiplatelet drugs like ticagrelor and prasugrel don’t rely on CYP2C19. They work faster, stronger, and aren’t affected by PPIs. That’s why the 2023 European Society of Cardiology guidelines now recommend ticagrelor as first-line for most heart attack patients.And there’s more on the horizon. Vonoprazan, a new acid blocker that doesn’t touch CYP2C19, is in late-stage trials. It could be the perfect replacement for PPIs in patients on clopidogrel - no interaction, no compromise.
For now, though, the answer is simple: if you need a PPI with clopidogrel, don’t take omeprazole or esomeprazole. Pick pantoprazole or rabeprazole. It’s not a guess. It’s based on years of data, real patient outcomes, and clear pharmacology.
What’s Still Unclear?
The biggest question remains: does this interaction actually lead to more heart attacks or deaths?Some large studies say no. Others say yes. The truth? It probably depends on you. If you’re a healthy 60-year-old with no other risks, maybe not. But if you’re older, diabetic, had a recent stent, or have kidney disease - that small drop in clopidogrel’s effect could be the difference between walking away and ending up back in the hospital.
That’s why doctors don’t just look at the drug interaction. They look at you. Your history. Your risks. Your meds. And they make a choice - not based on theory, but on what keeps you alive.
Can I take omeprazole with clopidogrel if I take them at different times of day?
No. Even if you space the doses 12 hours apart, omeprazole still blocks the enzyme (CYP2C19) your liver needs to activate clopidogrel. The inhibition lasts longer than the drug stays in your bloodstream, so timing doesn’t prevent the interaction. Switching to pantoprazole or rabeprazole is the only reliable solution.
Is pantoprazole really safe with clopidogrel?
Yes. Multiple studies, including meta-analyses from the NHS and European registries, show pantoprazole has no significant effect on clopidogrel’s antiplatelet activity. Its risk of heart events when taken with clopidogrel is nearly identical to taking clopidogrel alone (HR 0.98). It’s the preferred PPI in most clinical guidelines when both drugs are needed.
Do I need a PPI if I’m on clopidogrel?
Only if you’re at high risk for stomach bleeding. That includes being over 75, having a past ulcer, taking NSAIDs, or having H. pylori. For most people without these risks, the bleeding risk from clopidogrel alone is low, and adding a PPI offers little benefit. Always ask your doctor whether you truly need it.
What are the signs that clopidogrel isn’t working?
There are no obvious symptoms. Clopidogrel works silently to prevent clots. If it’s not working, the first sign might be a heart attack, stroke, or stent clot. That’s why doctors rely on lab tests like VASP or VerifyNow to measure platelet activity - not symptoms. If you’re concerned, ask your cardiologist about testing.
Are there alternatives to clopidogrel that don’t interact with PPIs?
Yes. Ticagrelor and prasugrel are newer antiplatelet drugs that don’t depend on CYP2C19 to work. They’re stronger, faster, and unaffected by PPIs. Many guidelines now recommend them over clopidogrel for patients with acute heart conditions. Ask your doctor if switching is right for you.
If you’re managing heart health with clopidogrel and a PPI, don’t assume all medications play nice together. The right choice can mean the difference between staying out of the hospital and ending up in one. Talk to your pharmacist. Ask your doctor. And make sure you’re not taking the wrong PPI - because when it comes to your heart, small details matter.

bhushan telavane
December 19, 2025 AT 06:17Just got prescribed clopidogrel last month and was on omeprazole for years. Had no idea this was a thing. Switched to pantoprazole after reading this-felt like I just dodged a bullet.
Connie Zehner
December 19, 2025 AT 08:37OMG I’M SO GLAD I READ THIS!!! 😭 I’ve been taking omeprazole with my stent meds for 3 years!!! My heart is literally screaming right now!!! 🚨💔
holly Sinclair
December 19, 2025 AT 10:30It’s fascinating how pharmacokinetics can quietly sabotage life-saving therapy without any overt warning. The CYP2C19 enzyme isn’t just a metabolic pathway-it’s a gatekeeper, and when you jam it with a PPI like omeprazole, you’re not just altering drug concentration, you’re altering biological destiny. The fact that this interaction has persisted in clinical practice despite robust evidence speaks to systemic inertia in medicine: we prioritize accessibility over precision, convenience over consequence. And yet, the human body doesn’t care about insurance formularies or OTC availability-it only responds to molecular reality. That’s why I’m not surprised that rabeprazole, with its negligible CYP2C19 inhibition, shows near-zero impact on platelet inhibition. The real tragedy isn’t the interaction-it’s how long it took for guidelines to catch up to the science.
mark shortus
December 20, 2025 AT 15:40OMG I CAN’T BELIEVE THIS IS STILL HAPPENING!!! 😱 I’m a nurse and I’ve seen THREE patients have stent thrombosis because their doctors didn’t know this!!! I screamed at my pharmacy last week when they tried to give me omeprazole with my Plavix-like, NO. JUST NO. I’M NOT DYING BECAUSE OF A $2 OTC DRUG!!!
Emily P
December 20, 2025 AT 18:27Is this real? I’ve been on clopidogrel since 2020 and just started pantoprazole last month. I’ve never felt better. I didn’t even know I was at risk. Thank you for this. I’m sharing it with my mom.
Vicki Belcher
December 21, 2025 AT 01:59YESSSSS this is so important!! 🙌 I’m a diabetic with a stent and was on omeprazole-switched to rabeprazole and my cardiologist said I’m now in the ‘low risk’ zone 🥹 Thank you for writing this like a human, not a textbook! ❤️
Jedidiah Massey
December 22, 2025 AT 02:59The CYP2C19 polymorphism landscape is non-trivial, and conflating pharmacodynamic interference with clinical endpoints is a classic reductionist fallacy. The COGENT trial’s null result is statistically underpowered for platelet reactivity endpoints-this is not evidence of safety, merely absence of statistical significance in a cohort not designed to detect it. The real-world data from the NHS registry, however, is compelling: HR 0.98 for pantoprazole versus placebo? That’s not noise-that’s clinical validation.
Lynsey Tyson
December 22, 2025 AT 04:12I get why doctors keep prescribing omeprazole-it’s cheap, it’s everywhere, and they’re trying to help. But I also get why patients end up in the ER. Maybe we need better labeling? Or a pop-up when doctors write scripts? I’m not mad, just… worried. Thanks for making this so clear.
Sarah McQuillan
December 23, 2025 AT 15:02Actually, I think this whole thing is overblown. I’ve been on omeprazole and clopidogrel for 8 years and I’m fine. Maybe the real problem is that people are too scared of their meds now? I mean, look at all this drama. My grandma took everything together and lived to 92. Maybe the science is just trying to sell us pricier pills.
anthony funes gomez
December 24, 2025 AT 09:17It’s not just CYP2C19 inhibition-it’s the kinetics of enzyme binding. Omeprazole’s sulfenamide derivative forms a covalent bond with the enzyme’s active site, irreversibly inhibiting it. The half-life of enzyme regeneration is ~24–48 hours. So even if you stagger doses, the enzyme pool remains suppressed. Rabeprazole’s lower binding affinity and faster clearance make it a kinetic outlier. The real takeaway? It’s not about timing. It’s about molecular architecture.
Alana Koerts
December 25, 2025 AT 22:16So what? People survive with this interaction all the time. The data is messy. The guidelines are conflicting. You’re scaring people for no reason. Also, pantoprazole causes vitamin B12 deficiency. Just sayin’.
Dikshita Mehta
December 27, 2025 AT 13:20As a pharmacist in Mumbai, I see this every day. Patients buy omeprazole from the corner shop and don’t tell their cardiologist. We’ve started putting stickers on clopidogrel bottles: ‘DO NOT MIX WITH OMEPRAZOLE.’ Simple. Effective. Saved at least 12 patients this year alone.
Nicole Rutherford
December 27, 2025 AT 21:22Of course you’re supposed to avoid omeprazole. But let’s be real-how many people even know what CYP2C19 is? Your average patient thinks ‘PPI’ means ‘stomach medicine.’ This isn’t a drug interaction-it’s a communication failure. And doctors? They’re overworked. They don’t have time to explain enzyme pathways. So blame the system, not the patient.
Mark Able
December 28, 2025 AT 05:44Wait, so if I take clopidogrel at night and PPI in the morning, it’s still bad? But I’ve been doing that for years! Are you telling me I’m gonna have a heart attack tomorrow? 😳