Corticosteroids for Autoimmune Disease: Benefits and Long-Term Side Effects
 Jan, 11 2026
Jan, 11 2026
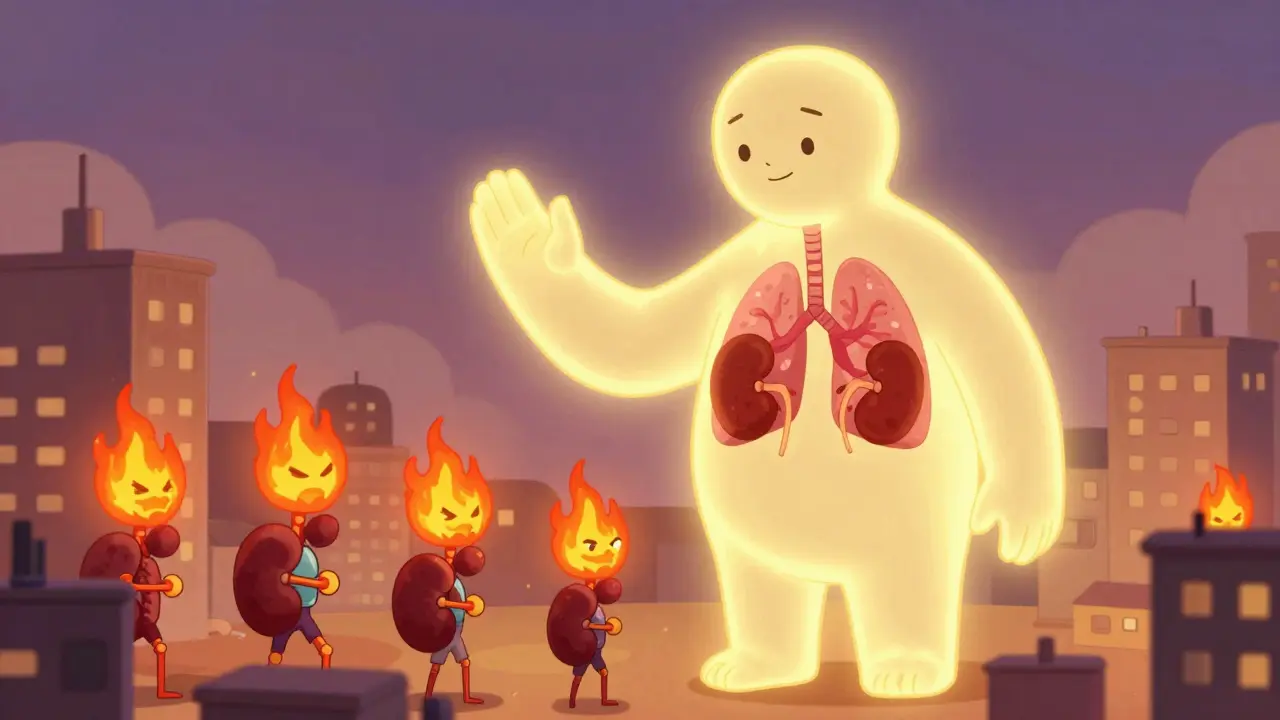
When your immune system turns against your own body, things get messy fast. Autoimmune diseases like rheumatoid arthritis, lupus, and vasculitis cause your body to attack healthy tissues, leading to pain, swelling, and organ damage. That’s where corticosteroids come in. These aren’t the bodybuilding steroids you hear about in sports news. These are powerful anti-inflammatory drugs that mimic cortisol, your body’s natural stress hormone. They work fast-sometimes in hours-and can stop a flare before it ruins your life.
How Corticosteroids Stop Autoimmune Flares
Corticosteroids like prednisone and methylprednisolone don’t just mask symptoms. They shut down the inflammation engine at the molecular level. Inside your cells, they bind to receptors that control gene activity. This turns off the genes that make inflammatory proteins like tumor necrosis factor-alpha and interleukins. They also block phospholipase A2, a key enzyme that starts the chain reaction of swelling and pain. The result? Less redness, less heat, less damage.
Unlike other immune drugs like methotrexate or azathioprine, which take weeks to kick in, corticosteroids work fast. That’s why they’re the first-line treatment for sudden flares. A patient with rapidly progressive kidney damage from vasculitis might get a daily IV dose of methylprednisolone to stop bleeding in the kidneys before other drugs even start working. In asthma or severe allergic reactions, a single oral dose can clear airway swelling in hours.
What Conditions Do They Actually Help?
Corticosteroids are used for a wide range of autoimmune conditions, but not all of them. They’re highly effective for:
- Rheumatoid arthritis (reducing joint swelling and pain)
- Systemic lupus erythematosus (controlling kidney and skin flares)
- Inflammatory bowel disease (Crohn’s and ulcerative colitis)
- Multiple sclerosis (reducing relapse severity)
- Autoimmune hemolytic anemia (when combined with rituximab)
- Psoriasis and severe skin rashes
- Goodpasture’s syndrome and polyarteritis nodosa
But they don’t work for everything. In advanced type 1 diabetes, where insulin-producing cells are already destroyed, corticosteroids won’t bring them back. Same goes for Hashimoto’s thyroiditis and Graves’ disease once the thyroid is severely damaged. In early stages of these diseases-when some cells are still alive-steroids might help slow the damage. But by the time symptoms are obvious, the window for steroids to make a difference is usually closed.
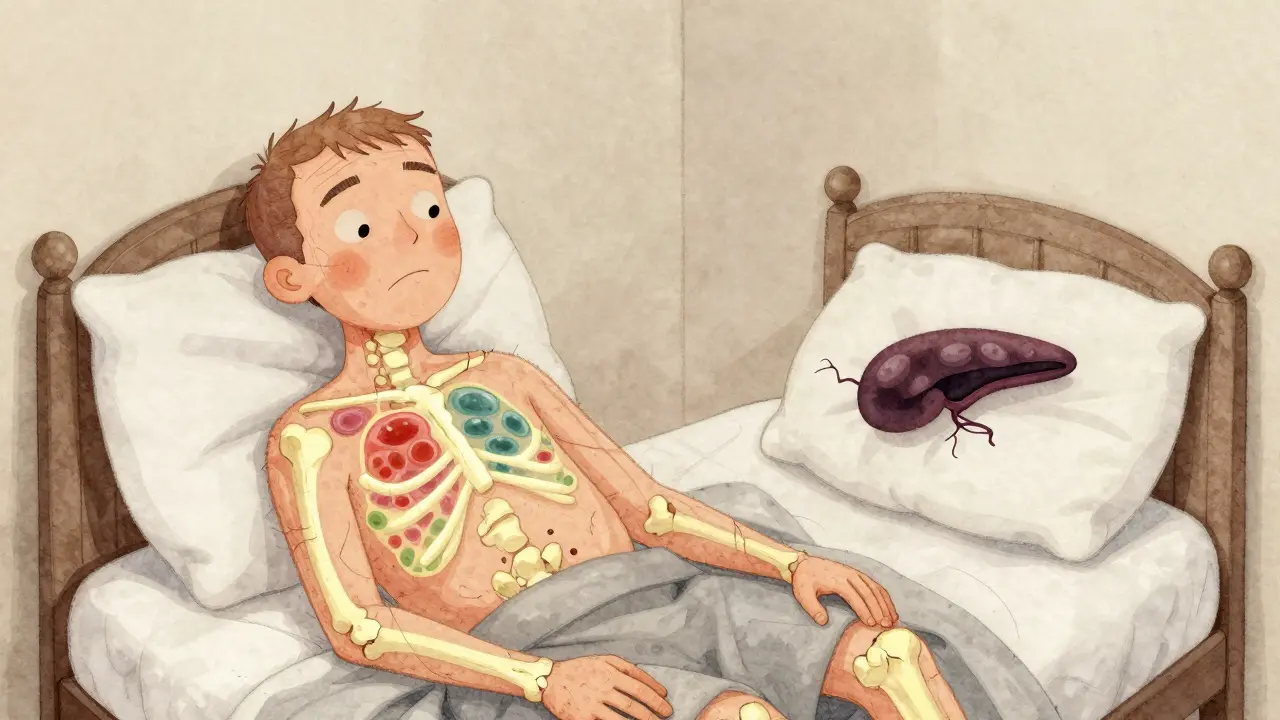
The Hidden Cost: Long-Term Side Effects
Here’s the catch: the longer you take corticosteroids, the more your body pays for the relief. That’s why doctors push to use the lowest dose for the shortest time possible.
One of the most serious risks is osteoporosis. Corticosteroids interfere with bone-building cells and increase calcium loss. Up to 40% of long-term users develop fractures, often without warning. That’s why anyone on steroids for more than three months gets a bone density scan and is put on calcium and vitamin D supplements-sometimes with bisphosphonates to protect the bones.
Cataracts are another common problem. After two years of daily use, the risk of clouded lenses jumps significantly. You might not notice it at first, but over time, vision gets blurry, glare worsens, and colors look faded. Surgery fixes it, but it’s avoidable if steroid use is kept minimal.
Your adrenal glands, which normally make cortisol, can shut down if you take steroids for too long. Your body thinks, “Why make our own when we’re getting a steady supply?” If you stop suddenly, your body can’t snap back. That’s adrenal insufficiency-and it’s dangerous. You could collapse from low blood pressure, nausea, and confusion. That’s why tapering off slowly is non-negotiable. Even after stopping, your adrenal glands may take months to wake up again.
Other side effects include:
- Weight gain, especially around the face and belly (moon face, buffalo hump)
- High blood sugar, sometimes triggering diabetes
- Mood swings, anxiety, or even psychosis in rare cases
- Thinner skin that bruises easily
- Increased risk of infections because your immune system is suppressed
- Sensitivity to sunlight and skin darkening
These aren’t rare side effects. They’re expected. That’s why doctors don’t just write a prescription and walk away. They monitor blood pressure, blood sugar, bone density, and eye health regularly.
How to Use Them Safely
There’s no magic trick to avoid side effects entirely. But you can reduce the risk dramatically.
Use the lowest effective dose. A 2023 study from the Australian Prescriber found that patients on 5 mg of prednisone daily had far fewer side effects than those on 10 mg or more-and still controlled their disease. Many people can stay stable on just 2.5 mg a day after the initial flare.
Take it in the morning. Your body naturally releases cortisol early in the day. Taking steroids around 7-8 a.m. mimics that rhythm and reduces the chance of adrenal suppression. Taking them at night? That’s a recipe for insomnia and hormonal chaos.
Combine with other drugs. Steroids are increasingly used as a bridge, not a lifetime solution. Once the flare is under control, doctors add methotrexate, azathioprine, or biologics like rituximab. These drugs take longer to work but have fewer long-term risks. In autoimmune hemolytic anemia, adding rituximab to prednisone doubled the time before relapse compared to steroids alone.
Protect your bones and eyes. Calcium (1200 mg), vitamin D (800-1000 IU), and weight-bearing exercise are essential. Get your eyes checked every year. If you’re on steroids for over a year, ask your doctor about a bone density scan.

The Future: Less Steroids, Better Outcomes
The goal now isn’t just to treat flares-it’s to get off steroids entirely. Newer drugs like biologics and JAK inhibitors are designed to target specific parts of the immune system without shutting down the whole thing. In lupus, drugs like belimumab have allowed many patients to cut their steroid dose in half or more.
Researchers are even looking at GILZ, a protein naturally triggered by corticosteroids that helps reduce inflammation. If they can create a drug that mimics GILZ without the side effects, it could replace steroids in the next decade.
For now, corticosteroids remain the fastest, most reliable tool we have to stop autoimmune flares. But they’re not a cure. They’re a fire extinguisher-not a way to stop the fire from starting again.
When to Talk to Your Doctor
If you’ve been on corticosteroids for more than three months, make sure you’re being monitored. Ask about:
- When you can start reducing your dose
- Whether you need a bone density scan
- If you should be on a bone-protecting medication
- Whether you’re a candidate for a steroid-sparing drug
- How to safely stop if your doctor recommends it
Don’t stop steroids on your own. Even if you feel fine, your body might still be depending on them. Sudden withdrawal can be life-threatening.
Are corticosteroids the same as anabolic steroids?
No. Anabolic steroids are used to build muscle and are often abused by athletes. Corticosteroids are anti-inflammatory drugs that suppress immune activity. They work on completely different pathways in the body and have very different uses and side effects.
Can corticosteroids cure autoimmune diseases?
No. Corticosteroids control symptoms and reduce inflammation, but they don’t fix the underlying immune dysfunction. Autoimmune diseases are chronic, meaning they last a lifetime. The goal is to manage them with the fewest side effects possible-not to cure them with steroids.
How long does it take for corticosteroids to start working?
You can feel the effects within hours to a few days. For severe flares, like in vasculitis or lupus nephritis, improvement in symptoms like joint pain or breathing difficulty is often noticeable within 24 to 48 hours. This rapid action is why they’re the go-to for emergencies.
What’s the safest way to stop taking corticosteroids?
Never stop abruptly. Your adrenal glands need time to restart cortisol production. Doctors create a tapering schedule, slowly lowering the dose over weeks or months. For people on high doses for over a year, tapering can take six months or longer. Blood tests may be used to check adrenal function before stopping completely.
Are there alternatives to corticosteroids for autoimmune diseases?
Yes. Drugs like methotrexate, azathioprine, and biologics (rituximab, belimumab, TNF inhibitors) are often used to reduce steroid dependence. These take longer to work but have better long-term safety profiles. Many patients now start with a steroid to control a flare, then switch to a steroid-sparing drug for ongoing management.
Can corticosteroids cause weight gain even if I eat healthy?
Yes. Corticosteroids change how your body stores fat and retains fluid. They increase appetite and shift fat to your face, neck, and abdomen-even if you’re eating the same amount. This isn’t about willpower; it’s a direct effect of the drug. Reducing the dose or switching to a steroid-sparing therapy is the only way to reverse it.
Is it safe to take corticosteroids during pregnancy?
Some corticosteroids, like prednisone, are considered relatively safe during pregnancy when used at low doses for necessary conditions like lupus or severe asthma. But they’re not risk-free. High doses may increase the chance of low birth weight or cleft palate. Always consult your doctor before continuing or starting steroids during pregnancy.

steve ker
January 12, 2026 AT 02:41Corticosteroids are just a bandaid for lazy medicine
George Bridges
January 12, 2026 AT 06:39I’ve seen friends go from active hikers to barely getting out of bed because of moon face and weight gain. It’s a tradeoff no one talks about until it’s too late.
Faith Wright
January 12, 2026 AT 12:34Oh so you mean like, the same drugs that turn your face into a balloon and your bones into chalk? Cool cool. Glad we’re all just vibing with osteoporosis and adrenal shutdown like it’s a wellness trend. 🙃
Bryan Wolfe
January 12, 2026 AT 22:12Hey everyone, I just want to say how important it is to remember that steroids are a bridge-not a destination!! I’ve been on them for 5 years with lupus, and switching to rituximab changed my life!! You CAN get off them!! Talk to your rheumatologist, get bone scans, take your calcium, and don’t give up!! You’re not alone!!
Christina Widodo
January 13, 2026 AT 10:01Wait so if I take prednisone for 3 months and then stop, my adrenals just... forget how to work? Like my body just deletes the cortisol app? That’s wild. So what happens if I get in a car crash after stopping? Do I just die?
Prachi Chauhan
January 15, 2026 AT 00:45steroids are like god's punishment for having a broken immune system. we are all just walking time bombs with moon faces. the body knows. it remembers. it waits.
Ben Kono
January 15, 2026 AT 02:10Why do doctors even prescribe these if they destroy your bones and make you fat and crazy I mean come on why not just give them a pill that makes you happy without turning you into a zombie
Cassie Widders
January 15, 2026 AT 12:33My mum was on prednisone for 7 years. She stopped cold turkey because she hated the face. Ended up in ER with low BP. Never talked about it again. Just… silent.
Konika Choudhury
January 17, 2026 AT 11:59India has better medicine than this why do we still use these ancient toxic drugs when we have ayurveda and yoga and turmeric
Darryl Perry
January 18, 2026 AT 11:12The data is clear. Long-term corticosteroid use correlates strongly with increased mortality. Prescribing them without mandatory bone density monitoring is negligent. This is not medicine. This is damage control.
Monica Puglia
January 19, 2026 AT 02:15My doctor put me on 5mg daily and I cried because I thought I’d be on it forever… then I found a support group. We do yoga, share recipes, and remind each other to take our D3. 💪❤️ You’re not broken. You’re adapting.
Cecelia Alta
January 20, 2026 AT 07:33Let’s be real - steroids are the villain origin story of every autoimmune patient. You go in for joint pain, you walk out looking like a cartoon villain with a buffalo hump and a face that could scare a toddler. And the worst part? Your doctor says ‘it’s temporary’ like that’s supposed to comfort you. Temporary. Right. Like ‘temporary’ unemployment. Like ‘temporary’ divorce. Like ‘temporary’ PTSD. Yeah. Right. I’ve been on it for 8 years. My bones are made of dust. My eyes are cloudy. And my kid doesn’t recognize me anymore. So no. I don’t ‘get it.’ I just survive it.
Rebekah Cobbson
January 21, 2026 AT 12:05Thank you for writing this so clearly. I just started tapering off after 2 years and I was terrified - but your point about morning dosing and combining with biologics? That’s exactly what my rheumatologist recommended. I’m not cured, but I’m finally feeling like me again. Keep sharing these truths.