Cost Sharing: Deductibles, Copays, and Coinsurance Explained for Medication Costs
 Feb, 15 2026
Feb, 15 2026
When you pick up your prescription, do you ever wonder why you paid $40 one month and $120 the next? It’s not because the price of the drug changed - it’s because of how your health insurance handles cost sharing. Deductibles, copays, and coinsurance aren’t just confusing terms thrown at you by insurance companies. They’re real numbers that directly affect how much you pay for your medications - and understanding them can save you hundreds, even thousands, of pounds a year.
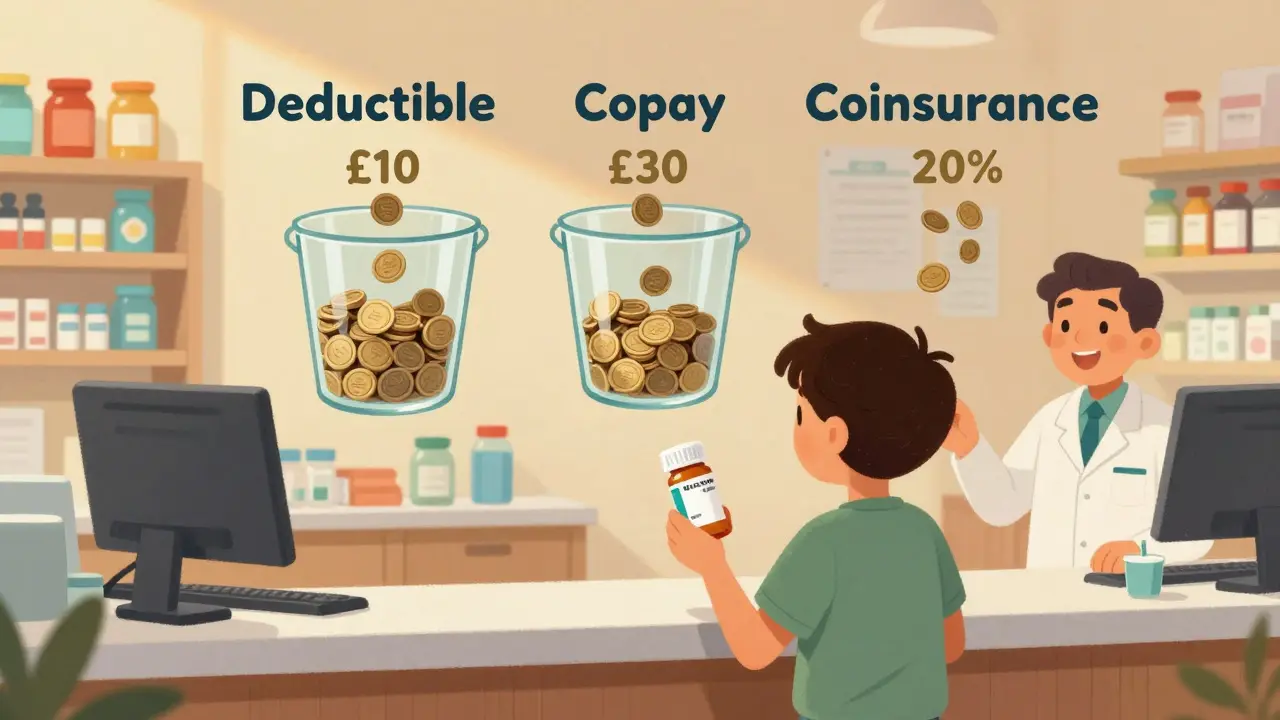
What Exactly Is Cost Sharing?
Cost sharing is the part of your healthcare bill that you pay out of your own pocket. Your insurance doesn’t cover everything. Even if you have a plan, you’re still responsible for a portion of the cost - and that portion depends on three things: your deductible, your copay, and your coinsurance. These three work together to split the cost between you and your insurer. The goal? To keep monthly premiums lower while making sure you don’t overuse care. But for people managing chronic conditions or taking expensive medications, this system can feel like a maze.
Deductible: The First Hurdle
Your deductible is the amount you pay each year before your insurance starts helping with costs. Think of it like a bucket. Every time you pay for a doctor’s visit, lab test, or prescription, that money goes into the bucket. Once the bucket is full - meaning you’ve paid your deductible - your insurance kicks in.
For example, if your plan has a $1,500 deductible, you pay 100% of your medication costs until you’ve spent that much. So if your monthly insulin costs £80, you’ll pay £960 in a year just to meet your deductible. After that, your plan starts paying a share. But here’s the catch: not all medications count toward your deductible the same way. Some plans treat prescriptions differently than doctor visits. Always check your plan’s Summary of Benefits to see which services count.
High-deductible plans (HDHPs) are common - especially in employer-sponsored insurance. In 2023, the average individual deductible was £1,945 (about $2,500). If you’re healthy and rarely take meds, these plans make sense. But if you’re on long-term medication, you’ll hit that deductible fast - and pay more upfront.
Copays: Fixed Fees at the Pharmacy
A copay is a fixed amount you pay each time you get a prescription filled. It doesn’t matter how much the drug costs. You pay £10, £20, or £30 - whatever your plan says - and your insurance covers the rest.
Most plans have different copay tiers based on the type of medication:
- Generic drugs: £10-£15
- Preferred brand-name drugs: £30-£50
- Non-preferred or specialty drugs: £75-£200+
Here’s the key: copays often apply after you meet your deductible - but not always. Some plans require you to pay the full cost of meds until your deductible is met, even if they have a copay. Others let you pay the copay right away, regardless of deductible. This varies by plan. Always ask your insurer: “Do I pay my copay before or after meeting my deductible?”
For someone taking a specialty drug like Humira or Enbrel, a £100 copay every month adds up to £1,200 a year - even after the deductible. That’s why knowing your tier matters. If your plan has a “preferred” list, ask your pharmacist if there’s a cheaper alternative that’s still covered.
Coinsurance: Paying a Percentage
Coinsurance is trickier because it’s not a fixed amount - it’s a percentage. After you meet your deductible, you pay a portion of the cost, and your insurance pays the rest. The most common split is 80/20: your insurer pays 80%, you pay 20%.
Let’s say your insulin costs £150 per month. After meeting your deductible, your coinsurance kicks in. You pay 20% of £150 = £30. Your insurance pays £120. Sounds fair? Until you realize that £150 isn’t the final price. That’s the “allowed amount” - what your insurer has negotiated with the pharmacy. If you go to an out-of-network pharmacy, the allowed amount might be £220. Now you’re paying 20% of £220 = £44. Suddenly, your monthly cost jumped by £14.
Coinsurance is especially important for expensive drugs. A cancer medication costing £5,000 per month? At 20% coinsurance, you pay £1,000. That’s £12,000 a year - and that’s before you hit your out-of-pocket maximum.

Out-of-Pocket Maximum: The Safety Net
This is the most important number on your plan. It’s the most you’ll pay in a year for covered services - including prescriptions. Once you hit it, your insurance pays 100% of all covered costs for the rest of the year.
In 2023, the federal cap was £7,300 for individuals and £14,600 for families (about $9,100 and $18,200). That means if you’re on a £1,200-a-month specialty drug, you’ll hit your max in about six months. After that, your meds are free.
But here’s the catch: only costs that count toward your deductible, copays, and coinsurance are included. Premiums don’t count. And if you go out-of-network, those costs might not count either - or they might count at a lower rate. Always check your plan’s fine print.
How These Three Work Together
Imagine you’re on a plan with:
- £2,000 deductible
- £30 copay for generics
- 30% coinsurance after deductible
- £7,300 out-of-pocket max
Month 1-6: You take a £100 generic drug. You pay £100 each month because you haven’t met your deductible. Total paid: £600.
Month 7: You hit your £2,000 deductible. Now your coinsurance applies. Same drug - £100. You pay 30% = £30. Insurance pays £70.
Month 8-12: You keep paying £30 per month. Total for the year: £600 (deductible) + £300 (coinsurance) = £900.
But if you take a £1,000 specialty drug? After deductible, you pay 30% = £300 per prescription. One prescription pushes you £300 toward your £7,300 max. Two more, and you’re halfway there.
This is why knowing your plan’s structure matters. A £30 copay sounds cheap - until you realize it doesn’t apply until after you’ve paid £2,000.
What’s New in 2026?
Since 2023, things have shifted. The Inflation Reduction Act capped insulin at £25 per month for Medicare patients - a huge relief for diabetics. But if you’re on private insurance, that cap doesn’t apply. Some private insurers have followed suit voluntarily, but not all.
Also, new transparency rules mean insurers must now show you estimated out-of-pocket costs for prescriptions before you fill them - online or via phone. Use it. Ask: “If I fill this today, how much will I pay?”
And remember: preventive care - like annual check-ups or vaccinations - still has no cost sharing. But prescriptions? Not always.
How to Save Money
- Use in-network pharmacies. Out-of-network means higher coinsurance or no coverage at all.
- Ask your doctor if there’s a generic or preferred brand on your plan’s formulary.
- Check if your insurer has a mail-order program - often cheaper for 90-day supplies.
- Use your plan’s cost estimator tool. Most insurers have one online.
- Review your plan’s Summary of Benefits every year. It’s required by law - and it’s written in plain language.
- If you’re on a high-deductible plan, consider an HSA. You can use pre-tax money to pay for meds, even before you meet your deductible.
One person in Bristol told me she switched from a £500/month specialty drug to a generic alternative after checking her plan’s formulary. Her out-of-pocket dropped from £150 to £15. That’s not luck - that’s knowing how cost sharing works.
Common Mistakes
- Thinking your premium counts toward your out-of-pocket max. It doesn’t.
- Assuming a copay applies immediately. Sometimes it doesn’t - until after your deductible.
- Not checking if your pharmacy is in-network. A quick Google search can save you hundreds.
- Ignoring the difference between “allowed amount” and “retail price.” Your insurance negotiates prices. You’re only responsible for a percentage of that negotiated rate.
Many people get hit with surprise bills because they didn’t check these basics. Don’t be one of them.
Do copays count toward my deductible?
It depends on your plan. Some plans count copays toward your deductible - others don’t. Most high-deductible plans require you to pay the full cost of prescriptions until you meet the deductible, even if you have a copay. Always check your plan’s Summary of Benefits or call your insurer directly.
What if I can’t afford my medication after meeting my deductible?
Many drug manufacturers offer patient assistance programs - especially for expensive medications. Nonprofits like the Patient Advocate Foundation and NeedyMeds can help you find discounts or free drugs. Also, ask your pharmacist about 30-day vs. 90-day supplies - sometimes buying more upfront lowers your per-month cost. And if you’re on Medicare, insulin is capped at £25 per month.
Why does my coinsurance change depending on where I fill my prescription?
Your insurance company negotiates prices with different pharmacies. If you use an out-of-network pharmacy, the “allowed amount” they’ve agreed on might be higher - or they might not cover it at all. That means you pay a percentage of a larger number, or pay the full retail price. Always use in-network pharmacies unless it’s an emergency.
Do preventive medications like birth control or vaccines count toward my deductible?
No. Under the Affordable Care Act, most preventive services - including birth control, vaccines, and annual check-ups - must be covered at 100% with no cost sharing, even if you haven’t met your deductible. But this only applies if the service is prescribed and billed as preventive. If your doctor prescribes a drug for a chronic condition, it may count. Always confirm with your insurer.
Can I change my plan to reduce medication costs?
Yes - during open enrollment (usually November to January), you can switch plans. Look for ones with lower coinsurance for your specific meds, or a lower tier for your drug class. If you have a life change - like a new diagnosis - you may qualify for a special enrollment period. Don’t wait until you’re hit with a £1,000 bill to act.
Final Tip
Don’t just accept your plan as it is. Every year, compare your medications to your plan’s formulary. Ask your pharmacist: “Is there a cheaper alternative that’s covered?” Call your insurer and say: “I take [drug name]. How much will I pay this year?” Write it down. You’ll be surprised how much you can save - and how little you actually need to pay.
