How to Compare Dissolution Profiles and What They Mean for Generic Drugs
 Jan, 23 2026
Jan, 23 2026
When you pick up a generic pill, you expect it to work just like the brand-name version. But how do regulators know it really does? The answer lies in something most people never hear about: dissolution profiles. These aren’t just lab curves on a graph-they’re the silent gatekeepers of generic drug safety and effectiveness.
What Dissolution Profiles Actually Measure
Dissolution testing watches how quickly a drug breaks down and dissolves in a liquid that mimics your stomach or intestines. It’s not about how fast the pill disappears-it’s about how fast the active ingredient gets released into solution. For a generic drug to be approved, its dissolution profile must match the brand-name drug’s under the same lab conditions.
Think of it like pouring two different brands of sugar into water. One dissolves in 30 seconds, the other in 2 minutes. Even if both are 100% sugar, the rate matters. With drugs, the speed of dissolution affects how fast the medicine enters your bloodstream-and whether it works the same way.
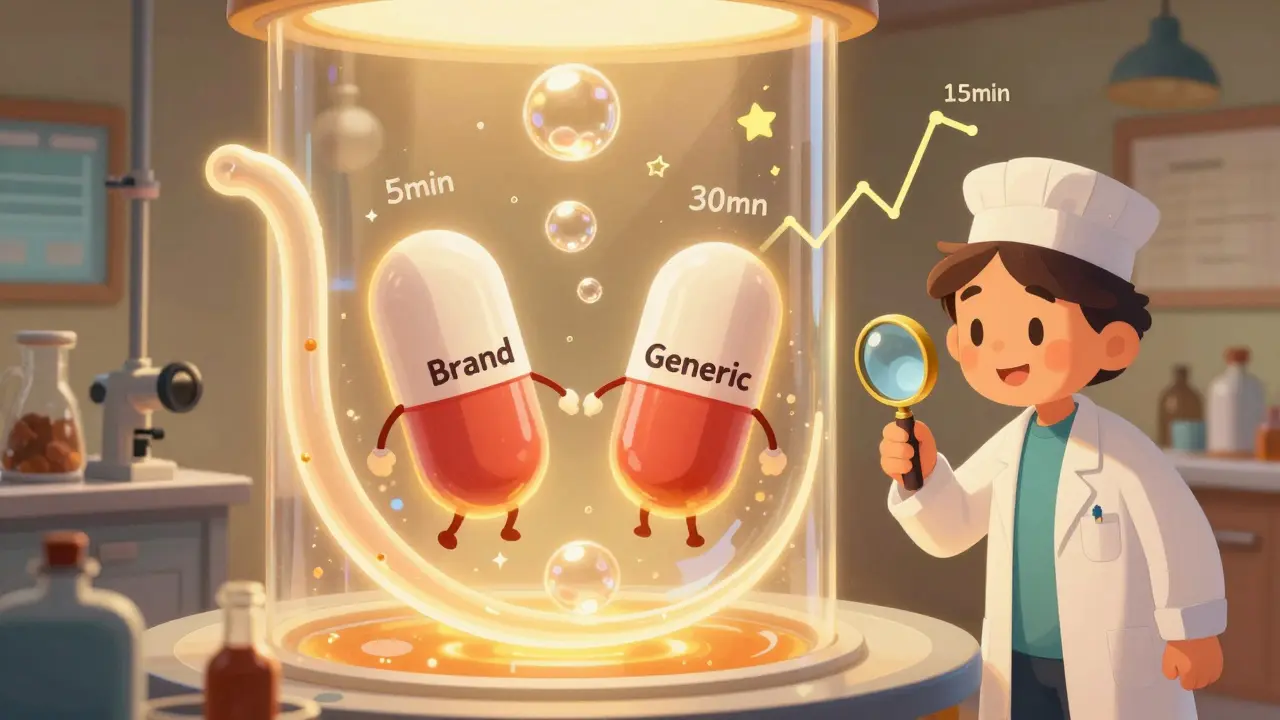
Regulators require testing 12 individual tablets or capsules for both the generic and brand-name versions. They use standardized machines (USP Apparatus 1 or 2), spinning at 50-100 rpm, at exactly 37°C, in fluids with pH levels matching your digestive tract. Time points are recorded every 5-15 minutes until at least 85% of the drug dissolves. The result? A curve showing percentage dissolved over time.
The f2 Factor: The Industry Standard for Comparison
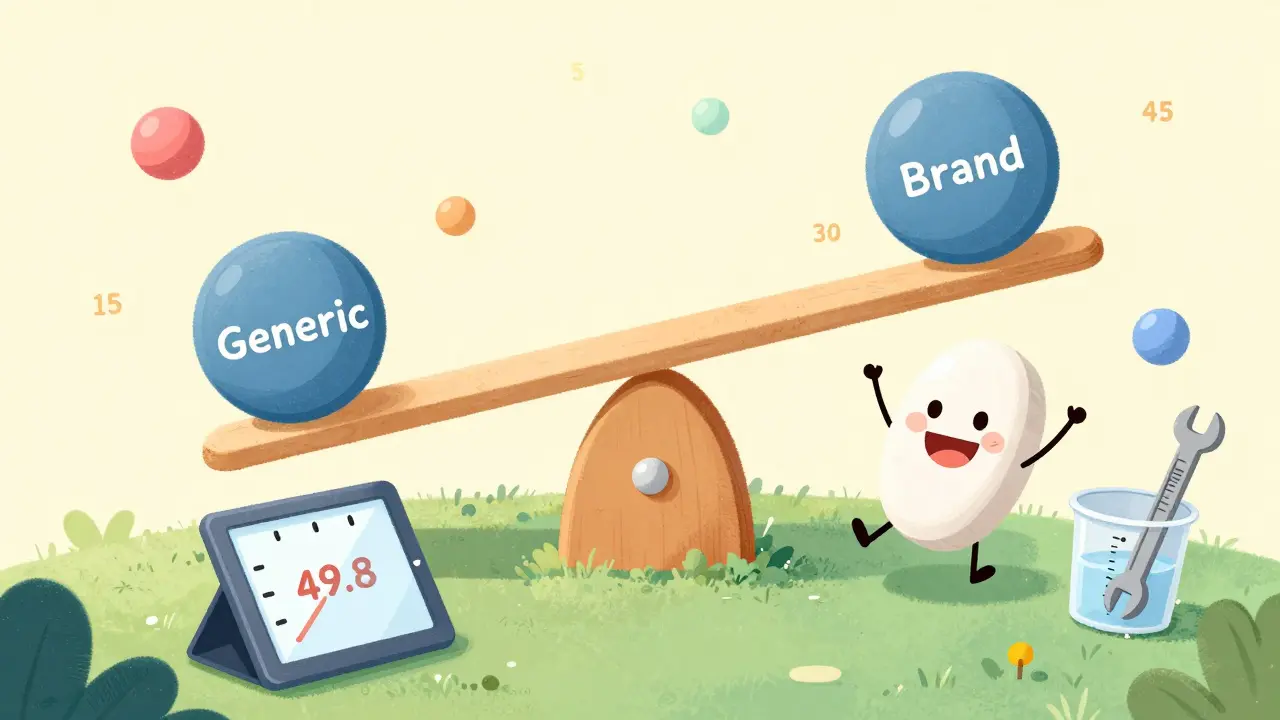
The most common way to compare these curves is using the f2 similarity factor. Developed in 1996 and now used in over 90% of FDA submissions, f2 is a mathematical formula that measures how close two dissolution profiles are. A perfect match gives you f2 = 100. The FDA accepts f2 values between 50 and 100 as evidence of similarity.
Here’s how it works: for each time point, the difference between the generic and brand-name dissolution percentages is squared. These squared differences are averaged, then plugged into a formula. The lower the average difference, the higher the f2 score.
But f2 isn’t magic. It has limits. If a drug dissolves too quickly-say, 80% in the first 15 minutes-small measurement errors can make f2 drop below 50, even if the drugs perform identically in the body. That’s why the FDA now recommends using f2 with other tools when dealing with highly soluble drugs. A 2022 survey found that 67% of labs struggled with f2 failures for fast-dissolving generics, not because the drugs were different, but because the test was too sensitive.
Why f2 Alone Isn’t Enough
Some experts argue that f2 is too blunt. It treats all time points equally, even though early dissolution (first 15 minutes) often matters more for how quickly a drug starts working. A generic could have the same total dissolution as the brand, but release 70% in the first 10 minutes while the brand releases 40%-and f2 might still say they’re similar. But that difference could mean the generic hits your bloodstream faster, which could be risky for drugs with narrow therapeutic windows, like warfarin or lithium.
Dr. Lawrence Yu, former FDA deputy director, put it plainly: “f2 > 50 is necessary but not sufficient.” The dissolution method itself must be able to tell the difference between good and bad batches. If your test can’t detect a crushed tablet or an overheated batch, it’s useless for quality control.
That’s why regulators now look at more than just f2. The area under the dissolution curve (AUC) is often added to the analysis. AUC measures total drug released over time. If the AUC ratio between generic and brand is between 0.80 and 1.25, and f2 is above 50, the chances of bioequivalence jump by 23% compared to using f2 alone.
When Dissolution Profiles Fail-and Why
Not every failed f2 means the generic is flawed. In fact, 73% of failed comparisons in a 2022 industry survey were due to lab error, not product differences. Common culprits:
- Calibration drift in dissolution apparatus
- Temperature fluctuations outside ±0.3°C
- Improper paddle alignment (wobble over 1mm)
- Wrong media volume (not enough to maintain “sink conditions”)
One Pfizer scientist shared on a pharma forum that his team once had to redesign a 25mg amlodipine tablet because f2 scored 49.8-despite identical clinical results. The fix? Adjusting the paddle height by 0.2mm and increasing media volume. The new f2: 63.2. Approval followed.
Low-dose drugs (under 5mg) are especially tricky. Tiny variations in tablet weight or mixing can throw off results. That’s why manufacturers often use more sensitive methods, like UV spectrophotometry with automated sampling, to reduce human error.
What Happens When Profiles Don’t Match
If f2 falls below 50 and AUC ratios are outside 0.80-1.25, regulators won’t approve the generic as bioequivalent. The manufacturer must either:
- Change the formulation (excipients, particle size, coating)
- Adjust the manufacturing process (compression force, granulation)
- Run a full bioequivalence study in humans (costing $1M-$3M and taking 6-12 months)
That’s why dissolution testing saves the industry billions. A 2021 study from the University of Maryland showed that using dissolution profiles instead of human trials cuts development costs by up to 60% and speeds approval by 12-18 months. For a generic company, that’s the difference between profit and loss.
Regulatory Differences Around the World
The FDA, EMA, and Health Canada all accept f2 ≥ 50, but their rules are tightening. In 2023, the FDA proposed tiered criteria: f2 ≥ 65 for drugs with narrow therapeutic indexes (like digoxin or cyclosporine), and f2 ≥ 50 for others. The EMA now requires 90% confidence intervals around each time point, not just a single f2 value.
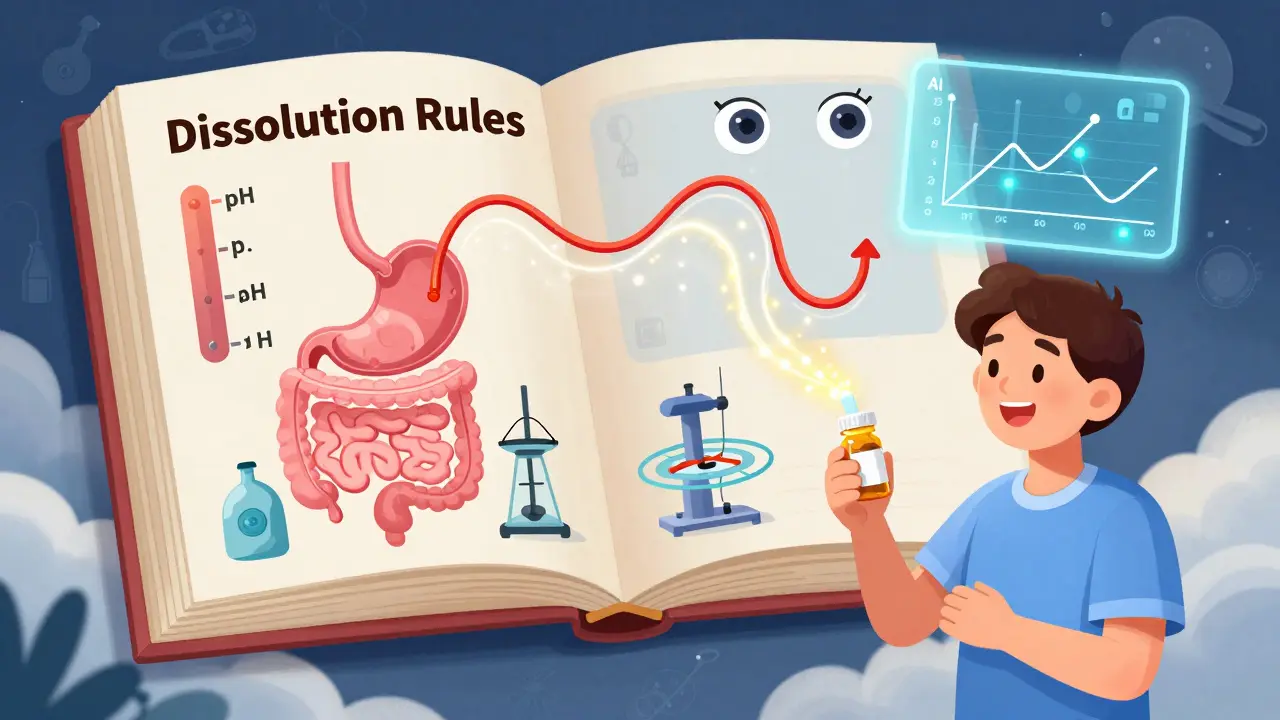
For BCS Class I drugs (highly soluble, highly permeable)-which make up 92% of biowaivers-dissolution must be tested in three pH levels: 1.2 (stomach), 4.5 (upper intestine), and 6.8 (lower intestine). The generic must pass f2 ≥ 60 in all three. For poorly soluble drugs (BCS Class II), surfactants are added to the media to mimic bile salts, ensuring the test reflects real digestion.
What This Means for You as a Patient
You don’t need to understand f2 scores to trust your generic. But knowing that regulators use these tests to ensure safety helps explain why generics are so much cheaper-and just as effective.
Every generic approved in the U.S. has passed dissolution testing against the brand-name drug. The FDA doesn’t approve a generic unless it dissolves the same way, under the same conditions. If your generic doesn’t work as expected, it’s likely due to individual body differences-not a failed test.
Still, if you’ve ever switched generics and felt a difference, you’re not imagining it. Some manufacturers use slightly different fillers or coatings that affect dissolution speed, even if they pass f2. That’s why some patients stick to one brand of generic. It’s not about safety-it’s about consistency.
The Future of Dissolution Testing
Researchers are now using AI to predict how a dissolution profile will behave in the body. Over a third of top pharma companies are testing machine learning models that analyze dissolution curves and predict bioavailability without human trials. Biorelevant media-fluids that mimic real stomach contents-are becoming standard for new drugs.
By 2026, the FDA and EMA plan to fully adopt these advanced methods. Dissolution testing won’t just be a gatekeeper-it’ll become a predictive tool. And for patients, that means even more confidence that your generic pill will do exactly what it’s supposed to.
What is the f2 similarity factor in dissolution testing?
The f2 similarity factor is a mathematical tool used to compare how similar two dissolution profiles are. It calculates the average difference between the percentage of drug dissolved over time for a generic and brand-name product. An f2 score between 50 and 100 is accepted by regulators as evidence of similarity, with 100 meaning the profiles are identical.
Why do some generics have different effects even if they pass dissolution tests?
Dissolution tests measure how fast the drug releases, but they don’t capture everything about how your body absorbs it. Factors like stomach pH, food intake, gut motility, and individual metabolism can cause slight differences in how a drug works. Some generics use different inactive ingredients that affect dissolution speed slightly-even within regulatory limits. If you notice a change after switching, talk to your pharmacist about sticking with the same manufacturer.
Can a generic drug fail dissolution testing and still be safe?
If a generic fails dissolution testing, it won’t be approved for sale. Regulators require dissolution similarity as proof of bioequivalence. A failed test means the drug may not dissolve at the same rate as the brand, which could lead to under- or over-dosing. There are no approved generics that failed dissolution testing-any that reach the market have passed.
Are dissolution tests the same for all types of pills?
No. Immediate-release tablets use standard conditions, but extended-release, delayed-release, or chewable tablets require different methods. For example, extended-release pills are tested over longer periods (up to 24 hours) with fewer time points. The FDA and EMA have specific guidelines for each dosage form, and the media used may include surfactants or enzymes to mimic real digestion.
How long does it take to develop a valid dissolution method?
Developing a reliable dissolution method typically takes 8 to 12 weeks. It involves testing across multiple pH levels, different agitation speeds, and stressed samples (like tablets that are overheated or under-compressed). The method must be able to detect even small differences in formulation. Only after validation can it be used for regulatory submissions.

Alexandra Enns
January 23, 2026 AT 21:20Wow, so you're telling me the entire generic drug system is just a glorified lab trick? I’ve been taking generics for years and now I’m supposed to believe some 50-100 f2 score means my blood isn’t getting screwed with? The FDA’s been cozy with Big Pharma since day one - this is just another way to greenlight cheap crap while pretending it’s safe. I’ve had generics that made me dizzy, others that did nothing - and you think a paddle spinning at 50 rpm is the whole story? LOL.
Marie-Pier D.
January 24, 2026 AT 08:24Thank you for breaking this down so clearly!! 🙏 I used to panic every time my pharmacy switched my generic, but now I get why it’s not always the drug - it’s the *method*. That paddle wobble detail? Mind blown. I’m gonna ask my pharmacist to tell me the manufacturer next time. Consistency > random chance, ya know? 💛
asa MNG
January 26, 2026 AT 08:22Sushrita Chakraborty
January 26, 2026 AT 12:05It is imperative to underscore that dissolution testing, while instrumental, constitutes only one facet of bioequivalence assessment. The regulatory frameworks of the FDA, EMA, and Health Canada are grounded in rigorous scientific methodology, and the f2 similarity factor, though imperfect, remains a validated statistical tool. Moreover, the inclusion of AUC and biorelevant media reflects a sophisticated, evolving understanding of pharmacokinetics.
It is unwise to conflate technical limitations with systemic corruption. The fact that 73% of failures stem from laboratory error underscores the necessity for standardization - not the invalidity of the system.
Dolores Rider
January 26, 2026 AT 14:24EVERYTHING about this is a lie. 🤫 The FDA doesn’t test the pills you take - they test the ones the company sends them. And guess what? The company knows exactly which batches to send. The real generics? The ones in your bottle? They’re made in a factory in China with different ingredients, different binders, and they’re tested in a lab that’s owned by the same parent company. They just tweak the paddle until the f2 hits 50.1 - and boom, approval. I’ve seen the emails. I’ve seen the redacted reports. You’re being used as a guinea pig.
Jenna Allison
January 28, 2026 AT 04:04Biggest thing people miss: f2 doesn’t care about the *shape* of the curve - just the average difference. So a generic could dump 80% in 10 minutes, then stall - and still get a 60 score if the brand did the same. But if you’re on a blood thinner? That spike could be dangerous. That’s why some docs tell you to stick with one brand of generic - not because it’s 'better,' but because the *pattern* is consistent. Your body learns the rhythm.
Also - yes, low-dose pills (under 5mg) are nightmares. A 0.5mg difference in weight? That’s a 10% dose error. No joke.
Sharon Biggins
January 29, 2026 AT 23:08I just wanted to say thank you for writing this. I’ve been a nurse for 18 years and I’ve seen patients panic when their generic changed - and honestly? Most of the time, it’s just anxiety. But your post helped me explain why it’s usually not the drug, it’s the *expectation*. I’m going to print this out for my patients. You made something dry actually helpful. 💕
John McGuirk
January 30, 2026 AT 04:44Let me guess - you think this is all legit? 😏 The dissolution tests? The f2 scores? The 'standardized machines'? Please. They use the same machines for all drugs - even ones that are supposed to be enteric-coated. Ever seen a pill that’s supposed to dissolve in the intestine? They test it in stomach fluid. That’s not science - that’s laziness. And don’t even get me started on how they pick the 'reference' brand. Sometimes it’s the *oldest* version - not the current one. They’re cooking the books.
Michael Camilleri
January 31, 2026 AT 04:57lorraine england
January 31, 2026 AT 18:08Okay but real talk - I switched from one generic to another last month and my anxiety spiked. Not placebo. I swear. I checked the manufacturer - different one. I called my pharmacy and they said 'same active ingredient.' But the fillers? The coating? That’s where the magic (or mess) happens. I’m going back to the old one. Not because it’s 'better' - just because my body knows it. Trust your gut. Or your stomach. Whichever.
Jamie Hooper
February 1, 2026 AT 22:06Husain Atther
February 3, 2026 AT 08:58This is an exceptionally well-structured exposition. As someone from India, where generic medicines serve as the primary healthcare access point for millions, I appreciate the nuance in acknowledging both the scientific rigor and the practical limitations. The point about low-dose drugs being especially vulnerable to manufacturing variance is critical - in our context, even minor inconsistencies can have disproportionate public health consequences. I hope regulators globally adopt tiered criteria for narrow-therapeutic-index drugs. Consistency saves lives.