How to Create a Family Overdose Emergency Plan for Medications
 Nov, 17 2025
Nov, 17 2025
Why Your Family Needs an Overdose Emergency Plan
Every year, over 100,000 people in the U.S. die from drug overdoses. Most of those deaths involve opioids - especially synthetic ones like fentanyl - and many happen at home. The truth is, if someone in your household takes prescription pain medication, you’re not immune. You might think, ‘That won’t happen to us,’ but the data doesn’t lie: 51.6 million U.S. adults got opioid prescriptions in 2022. And yet, only 12.3% of households have a plan in place for what to do if someone stops breathing.
This isn’t about fear. It’s about preparedness. Think of it like a fire extinguisher. You hope you never need it. But if you do, waiting to find one means losing precious minutes - and possibly a life.
Here’s the good news: if you act fast, you can save someone’s life. Naloxone, the overdose-reversing medication, works in 93% of cases when given in time. And it’s legal to carry and use in all 50 states. No matter who you are - parent, sibling, teenager, caregiver - you can learn how to respond. This plan isn’t complicated. But it only works if you build it before the emergency happens.
Step 1: Know Who’s at Risk and What Medications Are in the House
Start by listing every medication in your home that could cause an overdose. That includes prescription opioids like oxycodone, hydrocodone, fentanyl patches, and even benzodiazepines like Xanax or Valium. Don’t forget pills stored in bathroom cabinets, drawers, or old medicine bottles from past injuries.
Who’s at risk? Anyone taking opioids long-term, especially if they:
- Take more than prescribed
- Use alcohol or other drugs with their meds
- Have a history of substance use
- Are older or have breathing problems like COPD
It’s not just about addiction. People who take opioids for chronic pain can accidentally overdose if they miss a dose and then take extra later. Or if they switch to a stronger pill without realizing the dose changed. That’s why knowing what’s in your house matters.
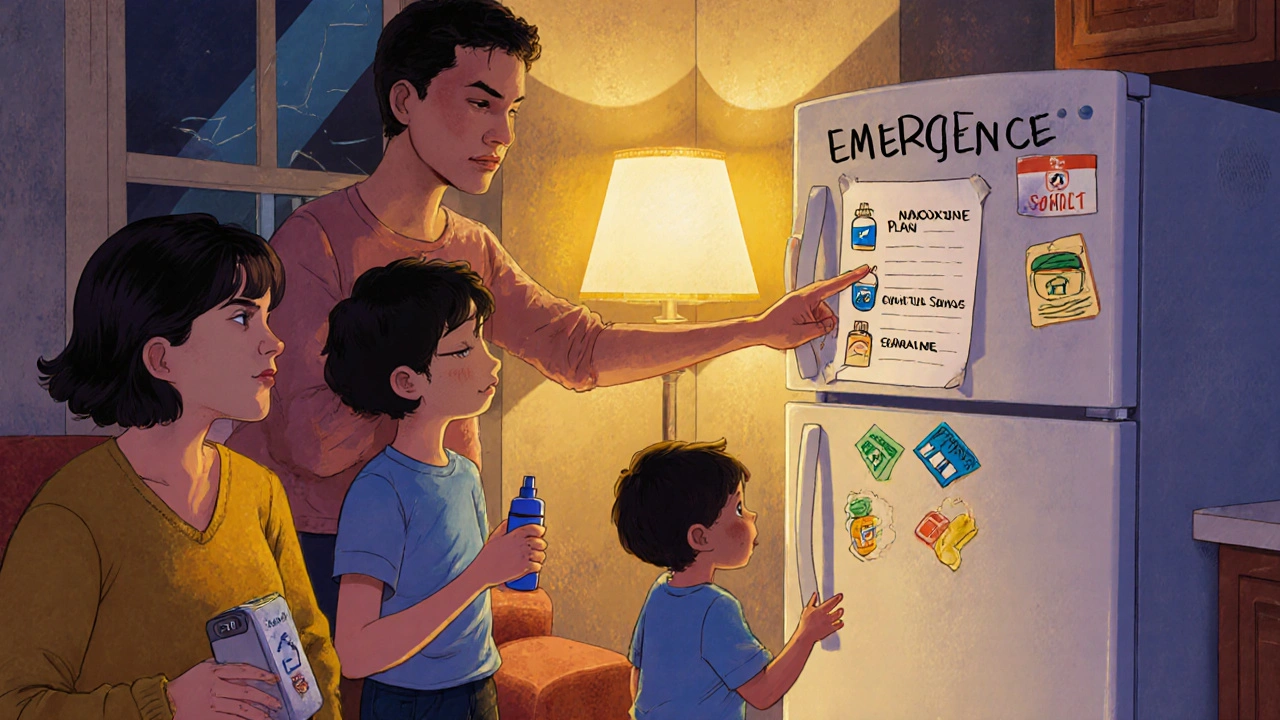
Write down each medication’s name, dose, and who it’s for. Keep this list in one place - maybe taped to the fridge or saved on your phone. If something happens, first responders will need this info fast.
Step 2: Get Naloxone - and Keep It Accessible
Naloxone (brand name Narcan) is the only medication that can reverse an opioid overdose. It’s safe, easy to use, and doesn’t work if someone hasn’t taken opioids. You can’t overdose on it. It won’t hurt someone who doesn’t need it.
You can get it without a prescription at most pharmacies in 46 states. Many CVS, Walgreens, and independent pharmacies offer it for $25 or less - especially with insurance. Thanks to the 2024 Inflation Reduction Act, Medicare Part D covers it with $0 copay. Some local health departments give it out for free.
Buy at least two doses. Fentanyl is so strong that one dose of naloxone often isn’t enough. Keep one in the kitchen, one in the bedroom, and maybe one in your car or purse. Don’t lock it away. Don’t hide it. Make sure everyone in the house knows where it is.
Check the expiration date every six months. Naloxone lasts 18-24 months, but heat and light can break it down. Store it at room temperature - not in the bathroom or near a window. If it’s expired, replace it. It’s not worth risking.
Step 3: Learn the Signs of an Overdose
An overdose doesn’t always look like what you see on TV. The person won’t necessarily be shaking or screaming. Often, they’re silent. Here’s what to look for:
- Unresponsive: Shout their name. Shake their shoulders hard. If they don’t wake up, it’s a red flag.
- Slow or stopped breathing: Count their breaths for 15 seconds. If they take fewer than 12 breaths per minute, or if their chest isn’t moving at all, they’re in trouble.
- Pinpoint pupils: Shine a light in their eye. If the black center is tiny like a pinprick, that’s a classic sign.
- Blue or gray lips/fingernails: This means their body isn’t getting enough oxygen.
Don’t wait for all these signs. If two are present, act. Fentanyl can knock someone out in under three minutes. Every second counts.
Step 4: Practice the Emergency Response
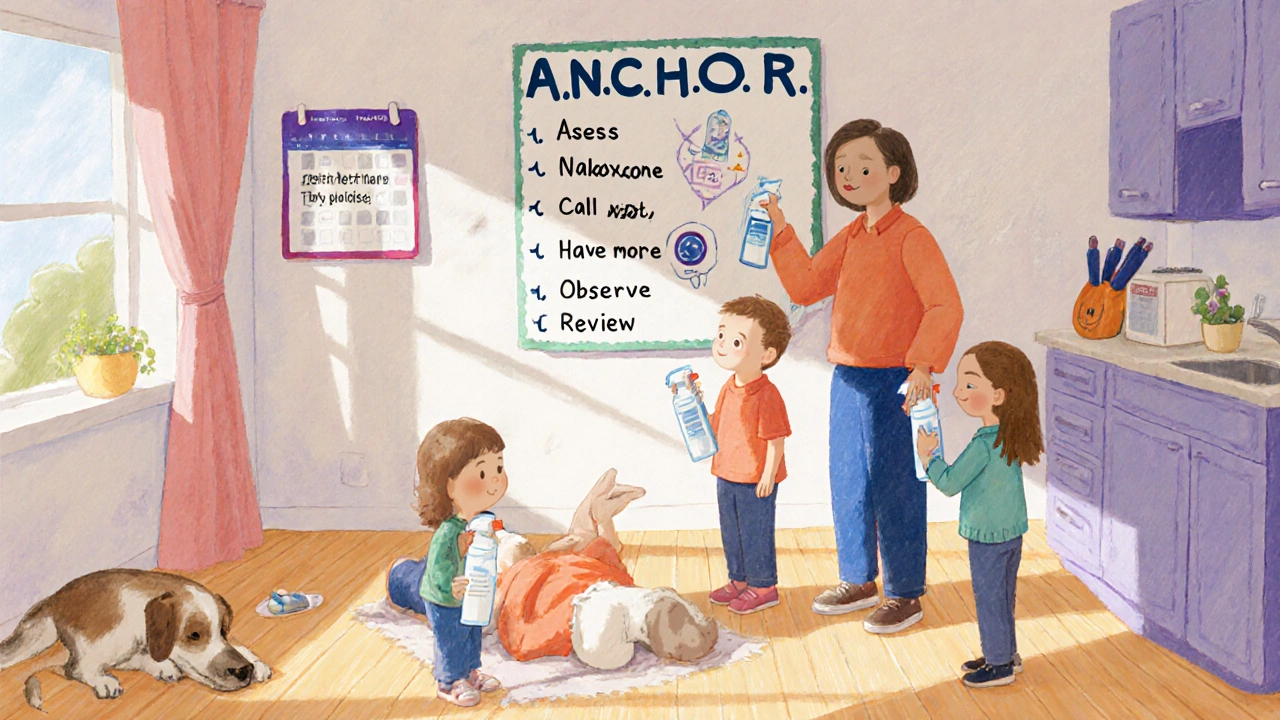
Here’s the exact sequence you need to follow - and you should practice it with everyone in the house:
- Assess: Check for responsiveness and breathing. If they’re not breathing or barely breathing, start the next steps immediately.
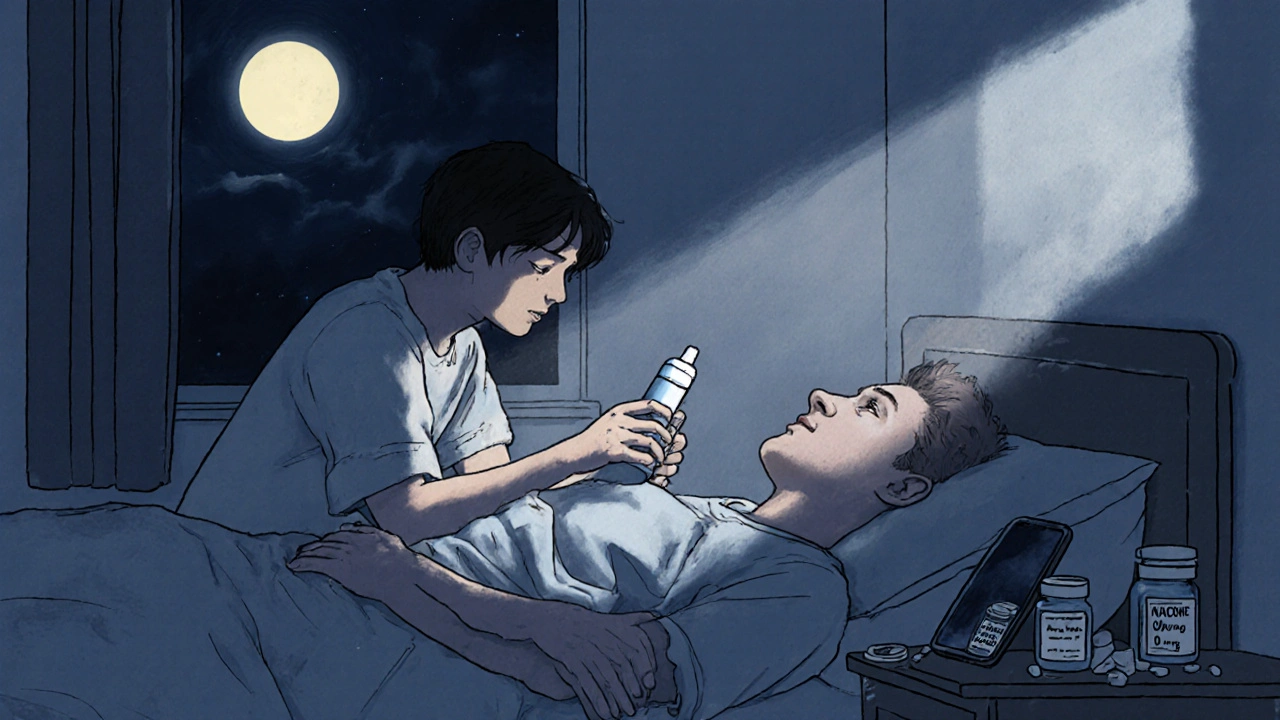
- Naloxone: Spray one dose into one nostril. If you’re using the injectable version, give it into the thigh muscle. Don’t waste time trying to find a vein.
- Call 911: Do this right after giving naloxone. Say, “Someone has overdosed on opioids. I’ve given naloxone.” Don’t wait to see if they wake up first.
- Have more ready: Keep the second dose nearby. If they don’t wake up in 3-5 minutes, give the second dose.
- Observe: Stay with them. Even if they wake up, they can slip back into overdose in the next 2-4 hours. This is called renarcotization. Don’t let them go to sleep.
- Review: After EMS arrives, talk to them. What happened? What meds were taken? This helps them treat the person better.
Use the A.N.C.H.O.R. method: Assess, Naloxone, Call 911, Have additional naloxone ready, Observe, Review. Memorize it. Write it on a card. Stick it to the fridge.
Step 5: Train Everyone - Including Kids
Don’t assume only adults will respond. Teens and even younger kids may be the first to find someone unresponsive. A 2023 survey found 34% of teens aged 14-17 know someone who’s overdosed. They need to know what to do.
Watch a 15-minute training video together. The American Red Cross has a free one online. Or find a local session through your health department. Practice on a mannequin or even a pillow - simulate spraying naloxone, calling 911, checking breathing.
Teach them: “If someone isn’t waking up, don’t panic. Don’t wait. Spray the nose. Call 911. Stay with them.”
Studies show families who train together retain the skills longer. One review found 94% of people who did in-person training could still do it correctly three months later. Those who didn’t? Only 52% could remember the steps.
What to Do After the Emergency
Surviving an overdose doesn’t mean the problem is over. Many people who get revived with naloxone go on to seek treatment. In fact, 89% of those who survive with help later connect with counseling or rehab services.
After the EMS leaves, talk to your loved one. Not in a blaming way. Say: “We were scared. We love you. We want to help.” Offer to go with them to a doctor, a support group, or a pain clinic.
Also, review your plan. Did everything go smoothly? Was the naloxone easy to find? Was the 911 call clear? Update your list. Replace used doses. Re-train everyone. This isn’t a one-time task. It’s an ongoing safety habit.
Common Mistakes and How to Avoid Them
People mean well - but mistakes cost lives. Here are the top errors families make:
- Waiting too long to call 911. The average family waits 6-8 minutes. Don’t wait for someone to wake up. Call immediately after giving naloxone.
- Using expired naloxone. 31% of failed attempts involved old kits. Check dates every six months.
- Not having enough doses. One spray often isn’t enough for fentanyl. Always keep two.
- Thinking naloxone is a cure. It saves lives, but it doesn’t fix addiction. Pair it with professional support.
- Keeping naloxone locked up. If it’s in a locked box, it’s useless in an emergency.
Don’t let embarrassment stop you. Talking about overdose is hard. But silence kills. The more you talk about it, the less scary it becomes.
Resources and Where to Get Help
You’re not alone. Many free tools and programs exist:
- Free naloxone kits: Many pharmacies, health departments, and community groups give them out for free. Search “free naloxone near me.”
- Training videos: American Red Cross, NIDA, and the NYC Health Department all offer free online courses.
- Apps: The “Overdose Guardian” app (released Jan 2024) sends alerts if someone in your ZIP code has an overdose - so you can be ready.
- Support: If you’re struggling with a loved one’s substance use, call the SAMHSA helpline at 1-800-662-HELP (4357). It’s free, confidential, and available 24/7.
Remember: You don’t need to be a doctor. You don’t need to be perfect. You just need to be ready.
Can I get naloxone without a prescription?
Yes. In 46 states, you can walk into a pharmacy and buy naloxone without a prescription. Many pharmacies, including CVS and Walgreens, offer it over the counter. Some even give it out for free through public health programs. Check with your local health department or use the Naloxone Finder tool online.
Will naloxone work on non-opioid overdoses?
No. Naloxone only reverses overdoses caused by opioids like heroin, fentanyl, oxycodone, or hydrocodone. It won’t work on overdoses from alcohol, benzodiazepines, cocaine, or other drugs. But if you’re unsure what was taken, give naloxone anyway. It’s safe and won’t harm someone who doesn’t need it.
Is it illegal to use naloxone on someone else?
No. All 50 states have Good Samaritan laws that protect anyone who gives naloxone in good faith during an emergency. You cannot be charged or sued for helping. These laws exist to encourage people to act without fear.
How long does naloxone last, and do I need to replace it?
Naloxone typically lasts 18-24 months if stored properly at room temperature and away from direct sunlight. Check the expiration date on the box. Replace it before it expires. If it’s been exposed to heat (like left in a hot car), replace it sooner. Never use expired naloxone - it may not work.
What if the person wakes up after naloxone? Do I still need to call 911?
Yes. Even if they wake up, you must call 911. Naloxone wears off in 30-90 minutes, but opioids can stay in the body much longer. This means the person can slip back into overdose - a condition called renarcotization. They need medical monitoring for at least 2-4 hours after the first dose.
Can I store naloxone in my car?
Yes - but be careful. Avoid storing it in places that get too hot, like the glove compartment in summer. If your car gets above 86°F, the medication can break down. Keep it in a cooler part of the car, like the door pocket, or bring it inside when possible. Always check the expiration date more often if it’s stored in a vehicle.
Next Steps: Build Your Plan Today
Don’t wait for a crisis to start planning. Right now, take five minutes:
- Find all medications in your home.
- Order two naloxone kits - one for home, one for your bag.
- Watch a 15-minute training video with your family.
- Write down your emergency steps and put them on the fridge.
- Set a calendar reminder to check expiration dates every six months.
This isn’t about predicting tragedy. It’s about making sure, if it happens, your family doesn’t freeze. You can be the difference between life and death. And you don’t need to be an expert to do it. Just be ready.

Jenny Lee
November 18, 2025 AT 14:37Evan Brady
November 19, 2025 AT 08:58Erica Lundy
November 20, 2025 AT 19:31Kevin Jones
November 22, 2025 AT 02:53Richard Couron
November 23, 2025 AT 14:57Alex Boozan
November 24, 2025 AT 01:17mithun mohanta
November 24, 2025 AT 02:33Ram tech
November 24, 2025 AT 03:27Alexis Paredes Gallego
November 24, 2025 AT 05:35Joshua Casella
November 25, 2025 AT 04:30Premanka Goswami
November 25, 2025 AT 21:08