Managing Diuretics and Hypokalemia in Heart Failure Patients: Practical Tips
 Nov, 7 2025
Nov, 7 2025
Hypokalemia Risk & Management Calculator
Calculate Your Potassium Risk
Your Results
When you have heart failure, your body holds onto too much fluid. That’s why doctors prescribe diuretics - pills that help you pee out the extra water. But here’s the catch: the same pills that relieve swelling can also drain your body of potassium. And when potassium drops too low - below 3.5 mmol/L - you’re at risk for dangerous heart rhythms, muscle weakness, and even sudden death. This isn’t rare. About 20-30% of heart failure patients on loop diuretics like furosemide or torsemide develop hypokalemia. It’s not just a side effect - it’s a warning sign that your treatment needs tuning.
Why Diuretics Lower Potassium
Loop diuretics work in the kidneys by blocking a specific transporter that moves sodium, potassium, and chloride out of the blood and into the urine. When that transporter is blocked, more sodium gets delivered to the lower parts of the kidney. There, it triggers the release of potassium into the urine. The result? You lose more water, but you also lose more potassium. The higher the dose of diuretic, the worse it gets. And if you’re on other meds like thiazides or laxatives, or if you’re not eating enough potassium-rich foods, the drop can be steep.What makes this even trickier is that your body adapts. After a few days on the same dose, your kidneys start reabsorbing sodium again - a phenomenon called within-dose diuretic tolerance. To keep pushing out fluid, doctors often increase the dose. But that means even more potassium gets flushed out. It’s a cycle: more diuretics → lower potassium → higher risk → more diuretics.
Why Low Potassium Is Dangerous in Heart Failure
Heart failure already strains your heart. The muscle is weaker, scarred, or enlarged. Low potassium makes it worse. Potassium helps your heart cells fire electrical signals properly. When levels fall below 3.5 mmol/L, those signals become erratic. That’s when dangerous arrhythmias - like ventricular tachycardia or torsades de pointes - can happen. Studies show that heart failure patients with potassium below 3.5 mmol/L have a 1.5 to 2 times higher risk of dying than those with normal levels.It’s not just about the number on the lab report. Many patients don’t feel symptoms until it’s too late. You might not notice muscle cramps or fatigue until your heart starts skipping beats. That’s why regular blood tests aren’t optional - they’re life-saving.
What the Guidelines Say
The 2022 AHA/ACC/HFSA guidelines are clear: monitor potassium closely. When you start a diuretic, check potassium within a week. After that, monthly checks are fine - unless something changes. If you’re hospitalized for worsening heart failure, check every 1-3 days. And if your potassium drops below 3.5 mmol/L, don’t wait. Act.The target? Keep potassium between 3.5 and 5.5 mmol/L. That’s the sweet spot: low enough to avoid fluid overload, high enough to protect your heart. The guidelines also stress that potassium levels should never be ignored just because you’re on other heart meds like ACE inhibitors or ARBs. Those drugs can raise potassium - but diuretics drag it down. It’s a balancing act.
How to Fix Low Potassium
There are three main ways to correct hypokalemia in heart failure patients:- Oral potassium supplements - For mild cases (3.0-3.5 mmol/L), 20-40 mmol of potassium chloride daily is usually enough. Take it with food to avoid stomach upset. Liquid forms work faster than tablets if you’re struggling to absorb pills.
- Intravenous potassium - If potassium drops below 3.0 mmol/L, or if you have symptoms like palpitations or muscle weakness, IV replacement is needed. Give it slowly - no more than 10-20 mmol per hour - and always with continuous ECG monitoring. Rapid IV potassium can stop your heart.
- Potassium-sparing diuretics - This is the game-changer. Adding a mineralocorticoid receptor antagonist (MRA) like spironolactone (12.5-25 mg daily) or eplerenone (25 mg daily) doesn’t just help potassium. It cuts your risk of dying by 30%, as shown in the landmark RALES trial. These drugs block aldosterone, the hormone that tells your kidneys to dump potassium. They’re now standard for heart failure with reduced ejection fraction (HFrEF).
Don’t just add potassium pills and call it a day. The goal is to reduce your reliance on potassium-wasting diuretics. That’s where newer treatments come in.
The Role of SGLT2 Inhibitors
In the last five years, SGLT2 inhibitors - drugs like empagliflozin and dapagliflozin - have changed heart failure treatment. Originally for diabetes, they’re now recommended for all heart failure patients, regardless of whether they have diabetes. Why? Because they help your kidneys remove fluid without pulling out potassium. In trials, they reduced diuretic doses by 20-30%. That means less potassium loss, fewer hospital visits, and lower death rates.They work by making your kidneys excrete sugar and sodium together - and potassium stays put. It’s a rare win-win. For patients stuck on high-dose diuretics and stuck with low potassium, adding an SGLT2 inhibitor can be the turning point.
What About Diet?
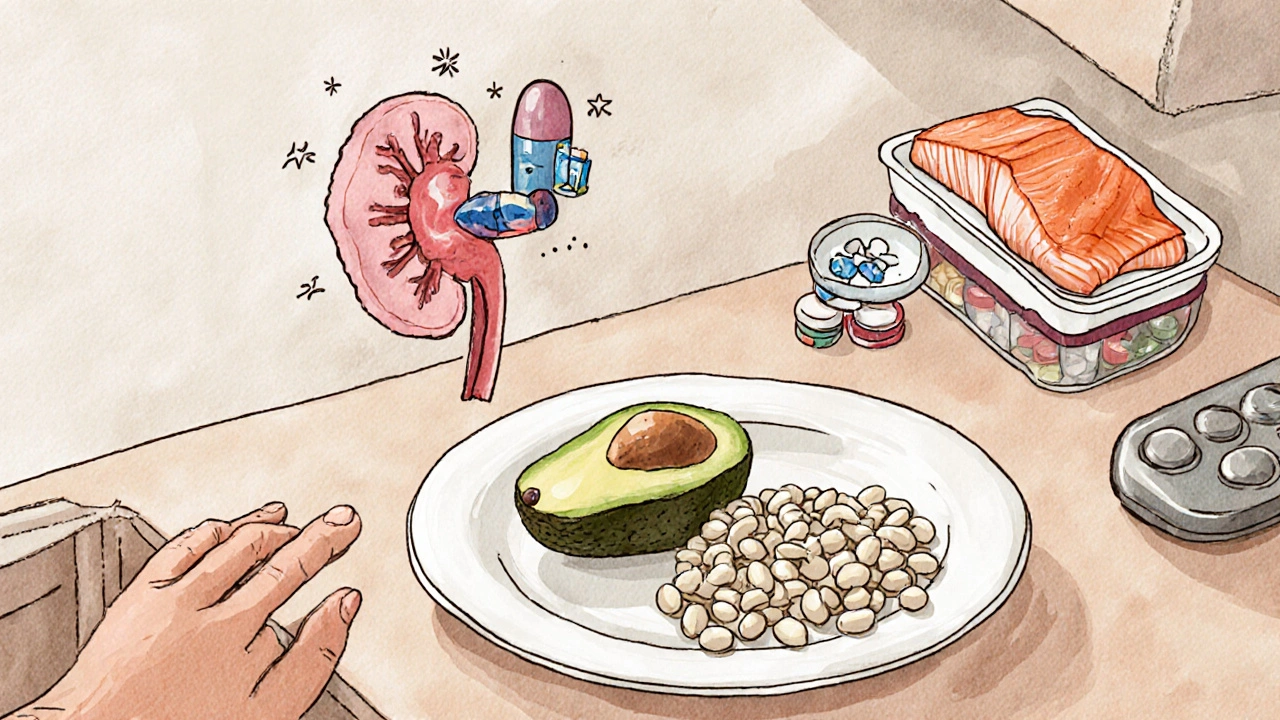
You’ve probably heard to eat more bananas, spinach, and potatoes. That’s true - but it’s not enough. You’d need to eat seven bananas a day to get 40 mmol of potassium. That’s unrealistic. Plus, heart failure patients are often told to limit salt - but cutting salt too hard can make potassium loss worse. When sodium drops, your body releases aldosterone, which makes your kidneys dump even more potassium.The fix? Don’t go overboard. Aim for 2-3 grams of sodium daily (80-120 mmol). That’s about one teaspoon of salt - not zero. Pair that with potassium-rich foods: lentils, avocado, white beans, yogurt, and salmon. But remember: food alone won’t fix a severe drop. It’s support, not a cure.

When to Use Thiazides or Extended-Release Diuretics
Some patients need more diuretic power than loop drugs alone can give. Adding a low-dose thiazide like metolazone (2.5-5 mg daily) can boost fluid removal - especially in patients with kidney problems. But here’s the risk: it makes hypokalemia worse. So if you add metolazone, you must also add an MRA.Another option? Extended-release furosemide. Regular furosemide peaks fast and wears off quickly, causing big swings in potassium. Extended-release versions smooth out the curve. They give steady diuresis over 12-24 hours, reducing the spikes and troughs that trigger potassium loss. This isn’t available everywhere yet - but where it is, it’s changing practice.
What to Avoid
- Skipping potassium checks - Even if you feel fine, check every month. - Overusing laxatives - Many patients use them for constipation from heart meds. But laxatives can cause massive potassium loss. - Stopping MRAs because of high potassium - If potassium rises above 5.5 mmol/L, don’t ditch spironolactone. Lower the dose. Add a binder. But don’t quit. The survival benefit is too big. - Using potassium supplements without medical advice - Too much potassium can be deadly, especially if your kidneys aren’t working well.Putting It All Together
Managing diuretics and hypokalemia isn’t about one magic pill. It’s about layers:- Start with the lowest effective diuretic dose.
- Add an MRA like spironolactone early - don’t wait for hypokalemia to happen.
- Consider an SGLT2 inhibitor - it reduces diuretic needs and protects the heart.
- Check potassium weekly at first, then monthly.
- Use oral potassium only for mild drops; IV for severe or symptomatic cases.
- Watch for hidden potassium thieves: laxatives, steroids, or high-dose thiazides.
- Don’t fear potassium - fear imbalance.
Heart failure management has moved far beyond just pushing out fluid. Today, it’s about protecting the heart’s rhythm, its muscle, and its future. Diuretics are still essential. But they’re no longer the whole story. The best outcomes come when you treat the whole patient - not just the swelling.
Can I just take potassium pills instead of changing my diuretics?
No. Potassium pills replace what you lose, but they don’t fix the root problem: too much potassium being flushed out. If you keep taking high doses of loop diuretics without adding a potassium-sparing agent like spironolactone, you’ll keep needing more pills. That’s not sustainable. The goal is to reduce potassium loss at the source, not just refill it.
How often should I get my potassium checked?
When you start or change a diuretic, check within 1 week. Once stable, monthly checks are enough. But if you’re hospitalized, have new symptoms like palpitations, or start a new medication like an SGLT2 inhibitor, check every 1-3 days until levels stabilize. Don’t wait for symptoms - low potassium often has none until it’s dangerous.
Is hypokalemia worse in heart failure with preserved ejection fraction (HFpEF)?
Yes - and it’s harder to manage. Patients with HFpEF often have more kidney problems and are more sensitive to fluid shifts. Aggressive diuresis doesn’t always help them, but it still causes potassium loss. Studies suggest these patients may need lower diuretic doses and earlier use of MRAs to avoid electrolyte crashes. Monitoring is even more critical.
Can I eat more potassium if I’m on an MRA?
Be careful. MRAs like spironolactone can raise potassium. If you’re already on one, eating huge amounts of potassium-rich foods (like salt substitutes or dried fruit) can push your levels too high. Aim for balanced intake - not extra. Your doctor will adjust your diet based on your blood tests.
Do SGLT2 inhibitors work for everyone with heart failure?
They work for most - including those with reduced or preserved ejection fraction, with or without diabetes. But they’re not for everyone. If you have very low kidney function (eGFR below 20), they may not work well. Also, they can cause genital infections or dehydration in older adults. Talk to your doctor about risks and benefits based on your specific situation.

Edward Weaver
November 9, 2025 AT 05:24Let me break this down for you non-med folks - diuretics are basically your body’s eviction notice for water, but they kick out potassium too. That’s like throwing out the baby with the bathwater, except the baby is your heart rhythm. You think eating a banana fixes it? Nah. You need MRAs - spironolactone isn’t optional, it’s the fucking backbone of modern HF care. Stop treating symptoms and start treating the damn system.
Lexi Brinkley
November 10, 2025 AT 04:06OMG YES THIS 😭 I had a cousin on furosemide who got admitted for VT because her K+ was 2.9… they didn’t check it for 3 months bc she ‘felt fine’… now she’s got an ICD and we all cry every time she eats a banana. MRAs aren’t ‘extra’ - they’re LIFE. 🙏
Kelsey Veg
November 10, 2025 AT 16:00ok but like… sgl2 inhibitors are kinda magic? i didnt even know they worked for hf without diabetes. my dr just threw empagliflozin at me and now i dont need my lasix as much. no more cramps, no more weird heart skips. its wild how one pill fixes like 3 problems at once. 🤯
Alex Harrison
November 12, 2025 AT 14:08I’ve been managing HF for 8 years and the biggest mistake I made was waiting until my potassium dropped below 3.0 before doing anything. Don’t wait. Start spironolactone early, even if your labs are normal. And yes, you need to check potassium monthly - no excuses. I missed one check and ended up in the ER. Don’t be me.
Jay Wallace
November 14, 2025 AT 02:32Let’s be clear: if you’re not using an MRA in HFrEF, you’re practicing 1990s medicine. And if you’re still relying on bananas to fix hypokalemia… well, you’re not just behind the curve - you’re on a different planet. The RALES trial was published in 1999. We’re in 2025. Do better.
Alyssa Fisher
November 15, 2025 AT 06:48It’s interesting how we treat the symptom (fluid overload) without addressing the mechanism (aldosterone-driven potassium loss). We’re so focused on pushing fluid out that we forget the heart needs electrolytes to beat - not just volume control. The real shift isn’t in the pills we add, it’s in how we think: from diuresis as the goal, to cardiac protection as the goal. That’s the paradigm.
Alyssa Salazar
November 15, 2025 AT 23:40Biggest red flag I see? Patients on metolazone without an MRA. That’s a potassium time bomb. You’re doubling down on the problem. And don’t even get me started on laxatives - I’ve seen people on 4 laxatives a day because they’re constipated from verapamil. You can’t out-eat potassium loss when you’re flushing it out like a toilet. Add the MRA. Period.
Beth Banham
November 16, 2025 AT 07:45I just started spironolactone last month. I was scared it would make me tired or give me boobs… but honestly? I feel more stable. My legs don’t swell as bad, and my heart doesn’t skip as much. I still eat my avocado. Still check my K+ monthly. Just… taking it slow. Grateful for the info here.
Brierly Davis
November 16, 2025 AT 14:19Just want to say - if you’re reading this and you’re scared to start an MRA or an SGLT2i, talk to your doc. Don’t let fear stop you. These aren’t risky - they’re life-extending. I’ve seen patients go from 3 hospitalizations a year to none after adding these. You’re not just managing HF - you’re reclaiming your life. Keep going.
Jim Oliver
November 18, 2025 AT 05:03Diuretics. Potassium. MRAs. SGLT2i. You’re all missing the point. The real problem? Doctors who don’t read guidelines. Or worse - patients who think ‘natural remedies’ fix electrolyte imbalances. You don’t cure hypokalemia with kale. You cure it with pharmacology. And if you’re still arguing about bananas? You’re not a patient. You’re a liability.