Medications with a Narrow Therapeutic Index: Why Expired Drugs Can Be Dangerous
 Nov, 20 2025
Nov, 20 2025
Some medications don’t just stop working after they expire-they can turn dangerous. This isn’t true for most pills in your medicine cabinet, but it’s a life-or-death concern for drugs with a narrow therapeutic index (NTI). These are the medicines where even a tiny change in dose or blood level can cause serious harm: a stroke, a seizure, internal bleeding, or even death. If you’re taking one of these drugs, the expiration date isn’t a suggestion. It’s a hard stop.
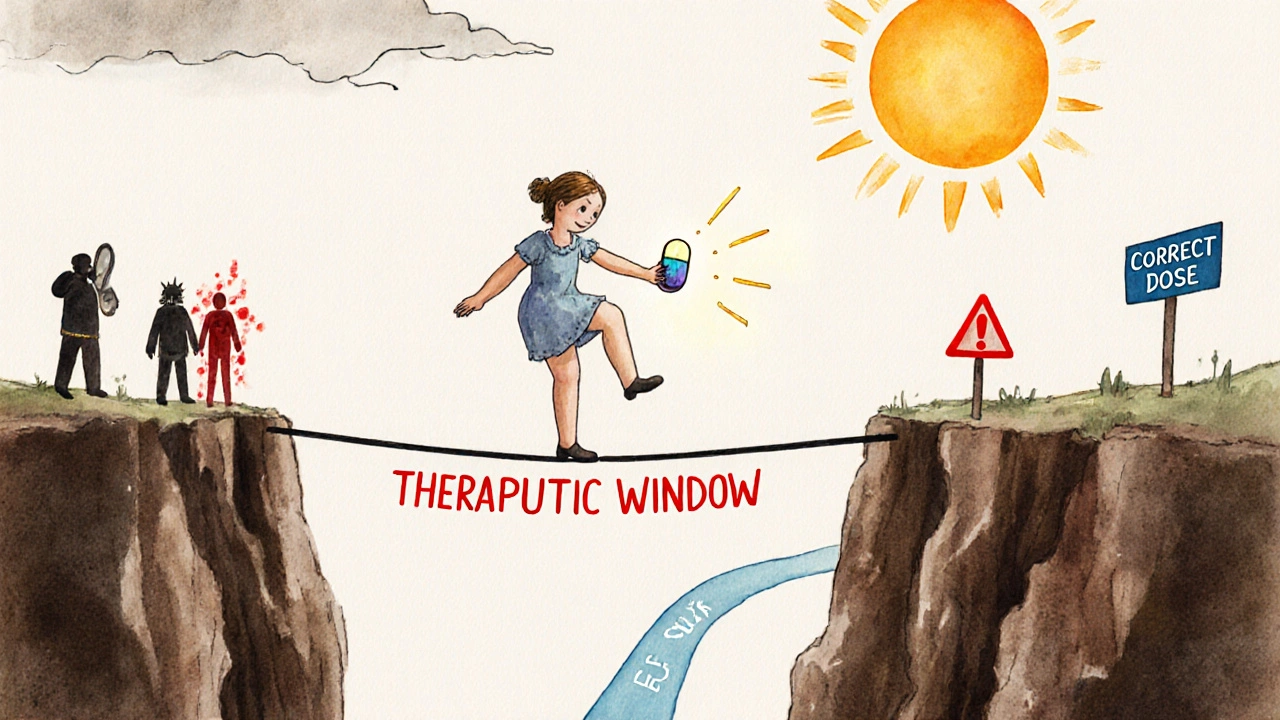
What Exactly Is a Narrow Therapeutic Index?
A narrow therapeutic index means the difference between a helpful dose and a toxic one is razor-thin. Think of it like walking a tightrope. One step too far, and you fall. For most drugs, your body can handle a little variation-you might take 10% more or less and still be fine. But for NTI drugs, that 10% could push you from safe to life-threatening.
The U.S. Food and Drug Administration (FDA) defines NTI drugs as those where small changes in blood concentration can lead to serious therapeutic failure or adverse reactions. The therapeutic window-the gap between the minimum effective dose and the minimum toxic dose-is less than twofold. In some cases, it’s barely 1.2 to 1.5 times. For example:
- Warfarin: A 10% increase in dose can spike your INR by 0.5 to 1.0, pushing you into dangerous bleeding territory.
- Digoxin: The safe range is 0.5 to 0.9 ng/mL. Toxicity starts above 1.2 ng/mL. That’s only a 33% increase from the top of the safe zone to the danger zone.
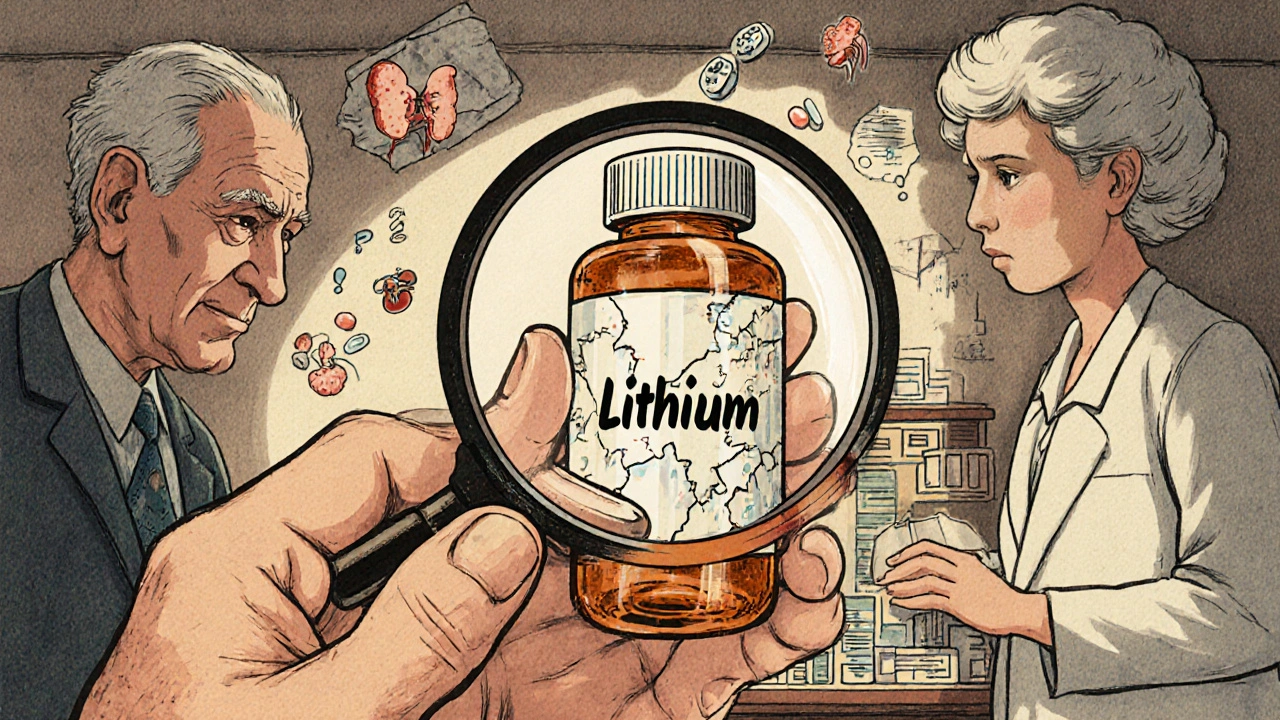
- Lithium: Used for bipolar disorder, it’s effective between 0.6 and 1.0 mEq/L. Above 1.5 mEq/L, you risk seizures, kidney damage, or coma.
These aren’t rare drugs. They’re commonly prescribed. If you or someone you know is on one of these, you’re already in a high-risk category.
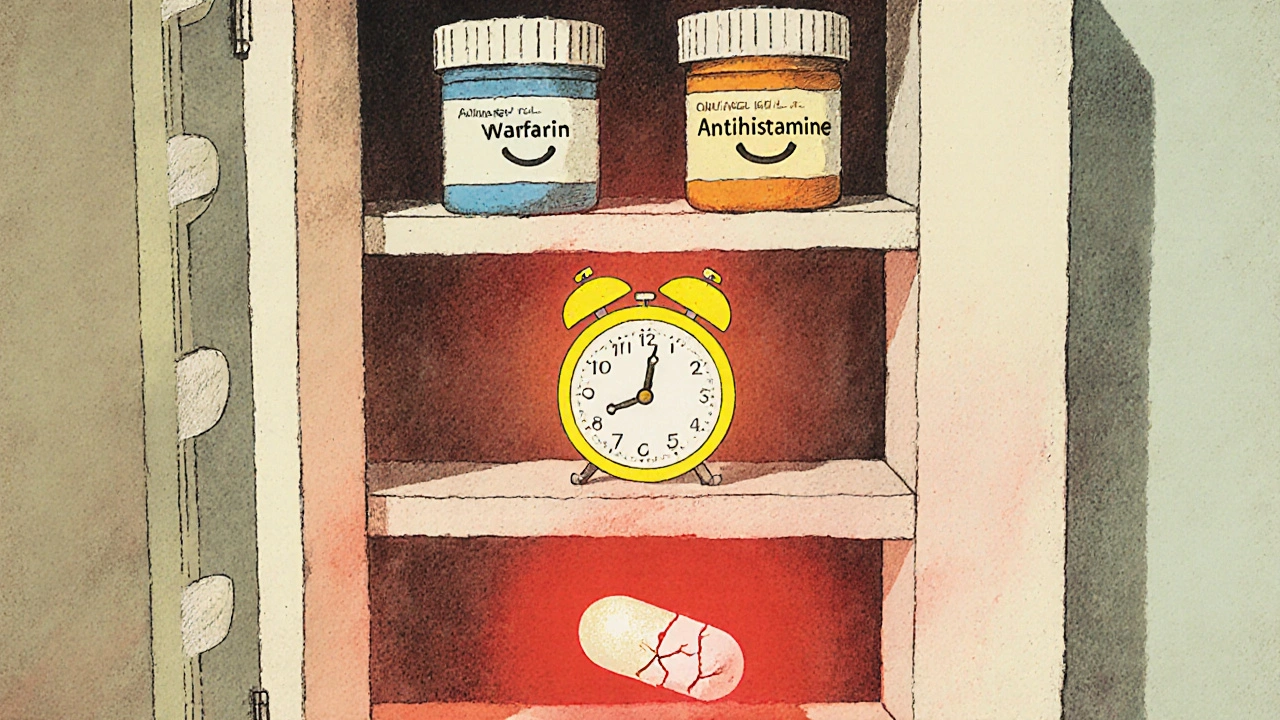
Why Expiration Dates Matter More for NTI Drugs
Most medications lose potency slowly. A 2012 FDA study found that over 90% of drugs remain stable for years past their expiration date-when stored properly. But that’s not true for NTI drugs.
Here’s why: if a regular painkiller loses 10% of its strength, you might just feel a little less relief. But if a warfarin tablet degrades by 10%, it could drop below the level needed to prevent a clot in someone with a mechanical heart valve. That’s not a missed dose-it’s a potential stroke waiting to happen.
Conversely, some drugs break down into harmful byproducts. While tetracycline is not an NTI drug, its degradation products can cause kidney damage. With NTI drugs, even minor chemical changes could shift the balance from therapeutic to toxic. There’s no safety buffer. No room for error.
The FDA requires stricter bioequivalence standards for generic NTI drugs-90% to 111% of the brand-name drug’s concentration, compared to the usual 80% to 125%. That means even tiny differences between brands or batches matter. Now imagine that same drug is old, stored in a hot bathroom, or exposed to moisture. The degradation could push it outside even that tight range.
Common NTI Drugs You Should Never Use After Expiration
Here are the most common NTI medications-and why you should toss them when they expire:
- Warfarin (Coumadin, Jantoven): Used to prevent clots. Even a small drop in potency can cause a clot. A small increase can cause internal bleeding. INR levels must stay between 2.0 and 3.0. Expiration = risk.
- Digoxin: Treats heart failure and irregular heartbeat. Toxicity can cause nausea, confusion, and fatal arrhythmias. The margin between safe and deadly is tiny.
- Lithium: Manages bipolar disorder. Blood levels must be precise. Too low: mood episodes return. Too high: tremors, confusion, kidney failure.
- Phenytoin (Dilantin): Controls seizures. Even a 15% drop can trigger breakthrough seizures. A 10% rise can cause dizziness, slurred speech, or coma.
- Levothyroxine: Replaces thyroid hormone. Small changes affect heart rate, weight, energy, and mood. Patients on this drug often need frequent blood tests-because even a 12.5 mcg difference matters.
- Carbamazepine (Tegretol): Used for epilepsy and nerve pain. Its metabolism varies widely between people. Expiration could alter absorption, leading to seizures or toxicity.
- Ciclosporin (Neoral, Sandimmune): Prevents organ rejection. Too little: rejection. Too much: kidney damage or cancer risk.
If you’re taking any of these, your pharmacist should flag them as high-alert medications. If they don’t, ask.
What Happens When You Take an Expired NTI Drug?
You might not notice anything right away. That’s the danger.
With warfarin, you might feel fine-until you bruise easily, or worse, bleed internally. With lithium, you might just feel tired or shaky, thinking it’s stress-until your kidneys start failing. With digoxin, you might get nausea, but dismiss it as the flu-until your heart goes into dangerous rhythm.
A 2014 study in the Journal of Clinical Pharmacy and Therapeutics found that drug-related problems with NTI medications were far more likely to cause hospitalization than those with other drugs. The risk isn’t theoretical. It’s documented in ER visits, ICU admissions, and death certificates.
There’s no reliable way to test if an expired NTI drug is still safe at home. No test strips, no home kits. You can’t measure blood levels without a lab. And even if the pill looks fine, the active ingredient may have degraded unevenly-some tablets in the bottle are weaker than others.
What Should You Do?
Follow these steps to stay safe:
- Check expiration dates monthly. Don’t wait until you run out. Mark your calendar to review your NTI meds every 30 days.
- Store them properly. Keep them in a cool, dry place-not the bathroom, not the dashboard of your car. Heat and moisture speed up degradation.
- Never use expired NTI drugs. Even if they’re only a month past the date. Don’t gamble with your life.
- Ask your pharmacist for a new prescription. Many insurance plans allow early refills for high-alert meds. Call ahead. Don’t wait until you’re out.
- Dispose of expired drugs safely. Use a drug take-back program. Don’t flush them or throw them in the trash. The FDA has a list of approved disposal locations.
Also, never switch brands or generics without your doctor’s approval. Even FDA-approved generics of NTI drugs can have slight differences in absorption. That’s why your doctor may insist you stay on the same brand.
Why Don’t We Know More About Expiration and NTI Drugs?
There’s a gap in the science. The FDA has strict rules for how generic NTI drugs must match brand-name versions-but no official studies look at what happens after expiration.
Manufacturers test stability for the labeled expiration date. After that? No legal requirement. Some companies test beyond expiration and find some NTI drugs remain stable for years. But that’s not guaranteed. And it’s not something you should rely on.
The American Society of Health-System Pharmacists and the Institute for Safe Medication Practices both say: treat NTI drugs like high-alert medications. That means assuming any change in formulation, storage, or age could compromise safety.
Until regulators require specific expiration stability data for NTI drugs, the safest rule is simple: if it’s expired, don’t take it.
What If You Accidentally Took an Expired NTI Drug?
If you took one dose of an expired NTI drug and feel fine, don’t panic-but don’t ignore it either.
- Call your doctor or pharmacist immediately.
- Don’t take another dose until you’ve spoken to a professional.
- If you’re on warfarin, get an INR test as soon as possible.
- If you’re on lithium or digoxin, watch for symptoms: nausea, dizziness, confusion, irregular heartbeat, tremors.
- Keep the bottle. Bring it to your appointment.
One mistake doesn’t mean disaster-but it does mean you need to act fast.
Bottom Line
NTI drugs aren’t like aspirin or antacids. They’re precision tools. A little too much, a little too little-and your body pays the price. Expiration dates exist for a reason. For these drugs, that reason is survival.
If you’re on one of these medications, treat every pill like it’s your last. Check dates. Store right. Replace early. Don’t wait for a crisis to realize you took a chance you couldn’t afford to take.
Your life isn’t worth the risk of saving a few dollars on a prescription.
Are all expired medications dangerous?
No. Most common medications like antibiotics, pain relievers, or allergy pills remain safe and effective for years after expiration if stored properly. But medications with a narrow therapeutic index-like warfarin, lithium, digoxin, or phenytoin-are an exception. Even small changes in potency can cause serious harm, so they should never be used past their expiration date.
Can I tell if an NTI drug has degraded just by looking at it?
No. Expired NTI drugs often look, smell, and taste the same. The active ingredient can break down without visible signs. A tablet may appear perfectly intact, but its potency could have dropped by 10% or more. You cannot rely on appearance to judge safety.
Why do some pharmacies refill NTI drugs early?
Because safety matters more than cost. Many insurance plans allow early refills for high-alert medications like warfarin or levothyroxine. Pharmacists and doctors know that running out or using an expired dose can lead to hospitalization. Early refills prevent dangerous gaps in therapy.
Is it safe to use a generic version of an NTI drug?
Yes-if it’s the same brand and you’re monitored closely. The FDA requires stricter bioequivalence testing for generic NTI drugs (90-111% potency match vs. 80-125% for most drugs). But even then, switching brands can cause changes in absorption. Always talk to your doctor before switching, and expect more frequent blood tests afterward.
What should I do if I can’t afford to replace my NTI medication?
Don’t skip doses or use expired pills. Talk to your pharmacist or doctor. Many drug manufacturers offer patient assistance programs. Nonprofits like NeedyMeds or RxAssist can help you find low-cost or free options. Your health isn’t a luxury-there are resources available.

Julia Strothers
November 21, 2025 AT 19:33So let me get this straight - the FDA lets drug companies slap an expiration date on life-or-death meds and then calls it a day? No follow-up? No long-term stability data? That’s not regulation, that’s corporate negligence wrapped in a white coat. I’ve seen warfarin bottles sitting in pharmacies for YEARS past expiry. And guess what? They still sell them. They don’t care if you bleed out as long as the profit margin stays clean. This isn’t medicine. It’s a lottery with your organs.
Erika Sta. Maria
November 23, 2025 AT 03:25ok but like… what if u just… take less? like if the pill is weak u just take 2? 😅 i mean its not rocket science? i read this one time on quora that expired aspirin turns into vinegar so maybe digoxin just turns into… i dunno… tea? 🫖
Nikhil Purohit
November 24, 2025 AT 15:12Hey, I’m on levothyroxine and this hit home. My pharmacist actually flagged my script as high-alert when I picked it up last month - didn’t even have to ask. She said if it’s expired by even a week, just get a new one. No drama, no guilt. I used to hoard pills ‘cause I’m cheap, but after reading this? Nah. My thyroid doesn’t negotiate. Thanks for the clarity.
Steve Harris
November 24, 2025 AT 23:51This is one of the most important public health pieces I’ve read in years. The distinction between general medications and NTI drugs is critical, and most people have no idea. The FDA’s 90–111% bioequivalence standard for NTI generics is often misunderstood - it’s not just about ‘same ingredients.’ It’s about absorption kinetics, particle size, fillers, and dissolution rates. Even tiny differences can cascade into clinical consequences. I’ve seen patients switch generics and end up in the ER because their INR went from 2.8 to 5.1 overnight. This isn’t theoretical. It’s daily practice in clinical pharmacy. Please, if you’re on one of these - don’t guess. Test. Monitor. Replace.
Elaina Cronin
November 26, 2025 AT 00:29While I appreciate the intent of this post, the tone borders on alarmist. Yes, NTI drugs require vigilance - but blanket statements like 'never use expired' ignore real-world access disparities. Many elderly patients in rural areas cannot afford frequent refills. The solution is not shaming, but systemic reform: subsidized access, mandatory pharmacy outreach, and government-backed stability testing for NTI generics beyond expiration. Until then, we must balance caution with compassion - not fear.
Willie Doherty
November 27, 2025 AT 14:15The cited 2012 FDA study on drug stability is frequently misapplied. It examined solid oral dosage forms under ideal storage conditions - not the humid bathroom cabinet where 78% of Americans store their meds. Furthermore, degradation kinetics are nonlinear. A 10% potency loss in warfarin may occur after 18 months, but the rate accelerates exponentially with heat exposure. The absence of regulatory data beyond expiration does not equate to safety. It equates to liability avoidance. The pharmacokinetic risk profile of NTI drugs demands a precautionary principle. I concur with the conclusion: discard. Do not gamble.
Darragh McNulty
November 28, 2025 AT 15:43Y’all need to chill 😅 I’m on lithium and I’ve had the same bottle for 2 years past expiry… still feels fine! 🤷♂️ But seriously - this is super important. My mom almost died when her digoxin got wet in the shower. Now I keep mine in a sealed container in the fridge. 🧊 Also - if you’re worried about cost, DM me. I work at a clinic and we have free samples. You’re not alone.
Cooper Long
November 29, 2025 AT 10:26Expiration dates are legal constructs not scientific absolutes. The military has stored NTI drugs for over a decade with no adverse events. The real issue is corporate control of pharmaceutical distribution. Why can’t we have national drug banks for expired but stable NTI medications? Why must profit dictate survival? The system is broken. The science is nuanced. The fear is manufactured.
Sheldon Bazinga
November 30, 2025 AT 23:37lol so u mean like if my warfarin is 3 months old i gotta go buy a new one? bro i got 3 kids and a 2000 dollar deductible. the pill still looks white and round. it dont smell like death. why are you all so extra? this is america not sweden. just take it. what’s gonna happen? u get a little bruise? big deal. #suckitup
Pravin Manani
December 2, 2025 AT 10:40From a clinical pharmacology standpoint, the real vulnerability lies in the polymorphic metabolism of NTI drugs - particularly CYP2C9 for warfarin and CYP3A4 for cyclosporin. Degradation doesn't just reduce potency; it alters metabolic pathways, potentially generating reactive intermediates that inhibit or induce enzyme activity. This creates a dual risk: subtherapeutic exposure AND unanticipated pharmacokinetic interactions. The expiration date isn't just about degradation - it's about the loss of predictable bioavailability. In patients on polypharmacy, this becomes a time bomb. Always verify with therapeutic drug monitoring. Never assume.