Methocarbamol and GI Side Effects: What You Need to Know
 Oct, 21 2025
Oct, 21 2025
Methocarbamol GI Side Effects Risk Calculator
Personal Risk Assessment
Answer a few questions to determine your risk level for GI side effects from Methocarbamol.
Risk Assessment Results
When to Seek Medical Help
Seek immediate medical attention if you experience severe vomiting, black/tarry stools, bright red blood, severe abdominal pain, or signs of dehydration.
Key Takeaways
- Methocarbamol can cause nausea, constipation, diarrhea, and abdominal discomfort.
- Elderly patients and those with pre‑existing GI conditions are most vulnerable.
- Concurrent use of NSAIDs, antacids, opioids, or alcohol can worsen stomach upset.
- Simple diet tweaks, proper hydration, and timing your dose can tame most symptoms.
- Seek medical help if you experience severe vomiting, bleeding, or persistent pain.
When you pick up a prescription for a muscle relaxant, the focus is usually on easing spasms. But a less‑talked‑about side of Methocarbamol is how it can stir up your stomach. If you’ve been warned about dizziness or drowsiness, you might be surprised to hear that nausea, constipation, or even diarrhea are fairly common. This guide walks through what the drug does to your gut, who’s most likely to feel the effects, and practical steps to keep your tummy happy while the medication does its job.
What is Methocarbamol?
Methocarbamol is a centrally acting muscle relaxant that reduces muscle spasms by depressing the central nervous system. It was first approved by the FDA in 1965 and is available as oral tablets, injectable forms, and extended‑release capsules. Doctors commonly prescribe it for acute low‑back pain, neck strains, and other musculoskeletal injuries where spasm relief can speed up rehab.
How Does Methocarbamol Work?
The exact mechanism isn’t fully mapped, but the drug blocks nerve impulses that cause involuntary muscle contraction. It’s metabolized primarily in the liver by the CYP2C19 enzyme, creating inactive metabolites that are cleared through the kidneys. Because its action is central rather than directly on the muscle fibers, side effects often show up in systems linked to the brain-drowsiness, light‑headedness, and the gastrointestinal (GI) upset we’re focusing on.
Typical Gastrointestinal Side Effects
Clinical trials and post‑marketing surveillance point to a handful of GI symptoms that appear in roughly 10‑20 % of users:
- Nausea and vomiting: Often mild and transient, but can become troublesome if you take the drug on an empty stomach.
- Constipation: Slowed gut motility is a known effect of many central‑acting agents.
- Diarrhea: A paradoxical reaction that may be linked to altered gut flora.
- Abdominal discomfort or cramping: Usually related to the drug’s effect on smooth muscle tone.
- Loss of appetite: Can compound the risk of malnutrition, especially in older adults.
Most of these issues resolve on their own within a week or two as your body adjusts. However, they can be a deal‑breaker for people who already struggle with digestive health.
Who Is at Higher Risk?
Not everyone gets a stomachache from Methocarbamol. Certain groups have a higher chance of experiencing GI trouble:
- Elderly patients: Age‑related slowdown of metabolism and existing constipation make them sensitive.
- People with a history of gastrointestinal disease (e.g., irritable bowel syndrome, ulcerative colitis, chronic gastritis).
- Individuals on multiple medications that irritate the lining of the stomach, such as non‑steroidal anti‑inflammatory drugs (NSAIDs).
- Patients who consume alcohol regularly; alcohol can amplify nausea and gastric irritation.
- Those with impaired liver function, because the drug’s breakdown via the CYP2C19 pathway is slower, leading to higher systemic levels.
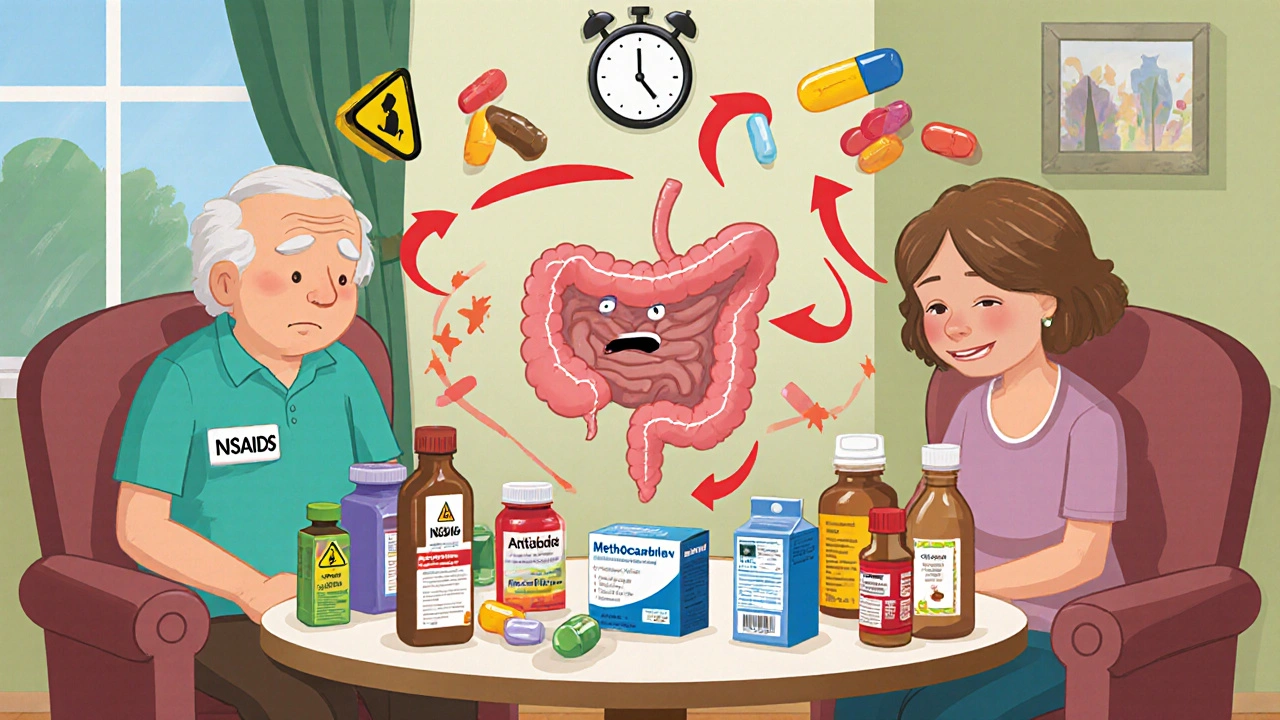
Drug Interactions That Worsen GI Issues
Some medicines share metabolic pathways or have additive effects on the gut. Knowing these combos can help you avoid a cascade of discomfort.
- NSAIDs (e.g., ibuprofen, naproxen): Both NSAIDs and Methocarbamol can irritate the stomach lining, raising the risk of gastritis or even bleeding.
- Antacids containing magnesium or aluminum: While they neutralize acid, they can also slow gastric emptying, worsening constipation.
- Opioids (e.g., oxycodone, tramadol): Opioids already cause constipating effects; adding Methocarbamol can make bowel movements painfully infrequent.
- Alcohol: Increases nausea, vomiting, and the chance of dizziness, making it harder to differentiate which drug is responsible.
- CYP2C19 inhibitors (e.g., fluoxetine, omeprazole): They raise Methocarbamol plasma levels, potentially intensifying all side effects, GI included.
Managing Gastrointestinal Side Effects
Before you toss the prescription, try these practical approaches:
- Take with food: A light snack or a full meal can cushion the stomach and reduce nausea.
- Hydrate wisely: Sip water throughout the day; avoid carbonated drinks that can bloat.
- Fiber boost: Whole grains, fruits, and vegetables help keep stools soft if constipation appears.
- Small, frequent meals: Rather than three large meals, aim for five to six smaller portions to keep gastric acidity stable.
- Adjust timing: If nighttime dosing makes you feel queasy, switch to a morning dose after breakfast.
- Review other meds: Discuss with your pharmacist whether an NSAID can be swapped for acetaminophen, or if a probiotic could offset diarrhea.
- Consider formulation: Extended‑release capsules dissolve slower and may produce milder GI upset compared to immediate‑release tablets.
If symptoms persist beyond two weeks, or if they become severe, contact your prescriber. Sometimes a different muscle relaxant with a lower GI profile is the better choice.
When to Seek Medical Help
Most stomach issues are uncomfortable but not dangerous. However, watch for red‑flag signs that demand immediate attention:
- Persistent vomiting that prevents you from keeping fluids down.
- Black, tarry stools or bright red blood - signs of gastrointestinal bleeding.
- Severe abdominal pain that doesn’t ease with over‑the‑counter antacids.
- Sudden, unexplained weight loss or loss of appetite lasting more than a week.
- Signs of dehydration: dry mouth, dizziness, reduced urine output.
These symptoms could indicate a more serious reaction or an underlying condition that needs treatment beyond adjusting the medication.
How Methocarbamol Stacks Up Against Other Muscle Relaxants
| Drug | Typical GI Side Effects | Incidence Rate | Notes |
|---|---|---|---|
| Methocarbamol | Nausea, constipation, diarrhea, abdominal discomfort | 10‑20 % | Central‑acting, short half‑life |
| Cyclobenzaprine | Dry mouth, constipation, mild nausea | 15‑25 % | Anticholinergic; higher sedation risk |
| Baclofen | Stomach cramps, constipation, occasional vomiting | 5‑15 % | GABA‑B agonist; may affect renal clearance |
Notice that while all three agents can cause constipation, Methocarbamol and Cyclobenzaprine share a slightly higher nausea rate. Baclofen’s GI profile is milder but can still be problematic for patients with existing bowel issues.
Bottom Line
If you’ve been prescribed Methocarbamol, keep an eye on how your stomach reacts, especially during the first two weeks. Simple measures-eating with the dose, staying hydrated, and avoiding alcohol-can prevent many uncomfortable episodes. Communicate openly with your doctor about any gastrointestinal trouble; a quick tweak in dosage or a switch to another muscle relaxant can make a big difference.

Can Methocarbamol cause severe stomach ulcers?
Methocarbamol isn’t classified as an ulcer‑causing drug, but its potential to irritate the stomach lining-especially when taken with NSAIDs or alcohol-can increase ulcer risk in susceptible individuals. If you have a history of ulcers, discuss alternative treatments with your clinician.
Is it safe to take Methocarbamol with antacids?
Occasional use of antacids for heartburn is generally fine, but magnesium‑based antacids can slow gastric emptying and worsen constipation. If you need regular antacid therapy, a calcium‑based product may be gentler.
How long does it take for GI side effects to subside?
Most patients notice improvement within 5‑7 days as the body adapts. If symptoms linger beyond two weeks, a dosage adjustment or medication change should be considered.
Should I stop Methocarbamol if I feel nauseous?
Don’t stop abruptly without medical advice. Try taking the dose with food, adjusting timing, or reducing the dose under supervision. If nausea is severe or persistent, contact your prescriber.
Can pregnancy affect Methocarbamol’s GI side effects?
Pregnancy can slow gastrointestinal motility, making constipation more common. If you’re pregnant or planning to become pregnant, discuss the risk‑benefit profile with your obstetrician.

Sakib Shaikh
October 21, 2025 AT 19:08Listen up, folks! Methocarbamol ain't just a muscle relaxer, it can turn your belly into a roller‑coaster.
Nausea hits you like a tsunami if you gulp it on an empty stomach, constipation sets in faster than a traffic jam in Delhi, and diarrhea will have you sprinting to the bathroom.
The key? Take it with a hearty breakfast, stay hydrated, and keep the NSAIDs on the shelf.
Trust me, I read the studies and the gastroinestinal side‑effects are real!
Ivan Laney
October 21, 2025 AT 20:06When examining the pharmacological profile of methocarbamol one quickly discovers that its central nervous system activity is not limited to muscle tone modulation.
The drug’s metabolism via CYP2C19 produces inactive metabolites that nonetheless linger long enough to irritate the gastric mucosa.
This irritation manifests as nausea, especially when the tablet dissolves in an empty stomach, a fact highlighted in multiple phase‑III trial reports.
Moreover, the agent’s influence on smooth muscle can decelerate intestinal transit, paving the way for constipation in susceptible individuals.
Conversely, a paradoxical up‑turn in gut flora sometimes triggers diarrhea, a side effect that confounds clinicians who expect only slowed motility.
Patients over the age of sixty are particularly vulnerable because age‑related hepatic decline amplifies systemic drug levels.
Co‑administration with non‑steroidal anti‑inflammatory drugs compounds the problem by further eroding the protective mucus layer of the stomach.
Alcohol, a well‑known gastric irritant, synergizes with methocarbamol to produce a crescendo of nausea and occasional vomiting.
Proton‑pump inhibitors such as omeprazole act as CYP2C19 inhibitors, unintentionally raising methocarbamol concentrations and intensifying all gastrointestinal complaints.
A practical mitigation strategy involves taking the medication with a moderate‑fat snack, which buffers the stomach lining and slows absorption.
Hydration cannot be overstated; sipping water throughout the day helps maintain lumen fluidity and eases the constipation burden.
Introducing soluble fiber-think oatmeal, bananas, or psyllium husk-provides bulk that counteracts the slowed peristalsis.
If diarrhea emerges, a short‑course probiotic containing Lactobacillus species may restore microbial balance without interfering with the primary therapy.
Should symptoms persist beyond a fortnight, clinicians frequently consider switching to baclofen or cyclobenzaprine, both of which have a slightly different GI side‑effect spectrum.
Ultimately, open communication with the prescriber ensures that dose adjustments or formulation changes, such as moving to extended‑release capsules, can be implemented before the patient experiences severe discomfort.
Vivian Annastasia
October 21, 2025 AT 21:30Great, another drug that makes your gut feel like a war zone.
John Price
October 21, 2025 AT 22:53If you can swallow it with a bite of toast, the nausea usually fades in a few days.
Nick M
October 22, 2025 AT 00:16Some claim the pharma giants hide the true constipation rates, but the data sheets still list a 10‑20 % incidence.
They say the side‑effects are “rare,” yet patients keep reporting bathroom battles.
Don’t trust the glossy pamphlets without digging into the original trial appendices.
eric smith
October 22, 2025 AT 01:40Interesting theory, but the FDA’s review documents are publicly accessible and they do acknowledge the rates.
It’s not a grand cover‑up, just a matter of statistical presentation.
Ericka Suarez
October 22, 2025 AT 03:03Believe it or not, that simple toast trick can be a lifesaver for many.
The carbohydrate load triggers insulin, which in turn can temper the nausea centers in the brain.
Pair it with a glass of water and you’ve got a mini‑buffer system against the drug’s harshness.
Just avoid heavy, greasy meals that could exacerbate the constipation.
Jake Hayes
October 22, 2025 AT 04:26Take methocarbamol with food and monitor for any persistent GI distress.
If symptoms exceed two weeks, consult your physician promptly.
parbat parbatzapada
October 22, 2025 AT 05:50Got it, I’ll keep an eye on my stomach.
Casey Cloud
October 22, 2025 AT 07:13Bottom line stay hydrated add fiber and don’t mix NSAIDs with this med
If you notice black stools or vomiting call your doctor right away
Most side effects settle within a week but you shouldn’t ignore them
Always discuss any other meds you’re on especially opioids or antacids
The goal is relief without turning your gut into a battlefield