Multiple System Atrophy: Understanding Parkinsonian Features and Survival Outlook
 Jan, 20 2026
Jan, 20 2026
Multiple System Atrophy (MSA) is not Parkinson’s disease. Even though it looks similar at first-slowness, stiffness, shaky movements-the truth is far more serious. MSA doesn’t just affect movement. It attacks the parts of your brain that control your heartbeat, bladder, digestion, and even breathing. And unlike Parkinson’s, it doesn’t respond well to the drugs that help millions. By the time most people get diagnosed, the damage is already widespread.
What Makes MSA-P Different From Parkinson’s?
The parkinsonian version, called MSA-P, makes up about two-thirds of all MSA cases. People with MSA-P have bradykinesia-movement that’s painfully slow-and stiff muscles that won’t bend easily. They shuffle when they walk. Their voice drops to a whisper. Their face loses expression, looking blank or mask-like. Tremors happen too, but they’re not the slow, rhythmic shakes you see in Parkinson’s. These are jerky, sudden tremors that show up when holding your arms out, not when they’re resting. The biggest clue that this isn’t Parkinson’s? Levodopa. That drug, which helps Parkinson’s patients move again, works for only 15 to 30% of MSA-P patients. And even when it does help, the benefit fades fast-usually within a year or two. If someone’s symptoms don’t improve after six months on high-dose levodopa, doctors start thinking MSA. That’s one of the first red flags.Autonomic Failure: The Silent Killer
While movement problems grab attention, it’s the autonomic system collapse that defines MSA-and shortens life. Nearly everyone with MSA-P develops orthostatic hypotension: their blood pressure crashes when they stand up. This isn’t just dizziness. It’s fainting spells, falls, and sometimes sudden loss of consciousness. About 90% of patients have this, and it often starts years before the shaking begins. Urinary problems are just as common. Eighty-five to ninety percent struggle with urgency, frequency, or complete incontinence. For men, erectile dysfunction is often the first sign-appearing 3 to 5 years before any movement issues. Sleep isn’t safe either. Eighty to ninety percent act out their dreams during REM sleep, kicking, yelling, even jumping out of bed. Sleep apnea, where breathing stops repeatedly at night, affects 60 to 70%. Temperature control fails too. Half of patients lose the ability to sweat in certain areas, making them prone to overheating. Digestion slows down. Bowel movements become infrequent and hard. All of this isn’t just inconvenient-it’s dangerous.How Fast Does MSA-P Progress?
MSA-P doesn’t wait. It moves fast. Within 1 to 2 years of symptoms starting, 85% of patients have already had a fall. By 3.5 years, most need a cane or walker. By 5.3 years, they’re in a wheelchair. And by 5 years, half have lost nearly all their ability to move independently. The median survival time? Just 6 to 10 years from when symptoms first appear. Five years after diagnosis, only about 60% are still alive. By ten years, that number drops to under 20%. The most common causes of death? Pneumonia from swallowing problems, respiratory failure, or sudden cardiac arrest. MSA-P declines faster than the cerebellar type (MSA-C). People with MSA-P reach the most advanced stage-bedridden or wheelchair-bound-in about 5.7 years on average. For MSA-C, it takes nearly three years longer. And if levodopa doesn’t help at all, survival drops to around 6.2 years. If there’s even a small improvement, it extends to nearly 10.
Why Is Diagnosis So Hard?
Early on, MSA-P looks exactly like Parkinson’s. Even neurologists can’t tell the difference for the first few years. That’s why misdiagnosis is common. The real clues come later: severe autonomic symptoms appearing within 3 years of movement problems, poor response to levodopa, and specific brain changes on MRI. One telltale sign is the “hot cross bun” sign-a cross-shaped pattern on MRI scans of the brainstem. It shows up in about half to 80% of MSA-C cases, but can also appear in MSA-P. Another is shrinkage and darkening of the putamen, a brain region involved in movement control. These signs don’t show up right away. That’s why diagnosis accuracy only hits 85 to 90% after 3 to 5 years. Dr. Gregor K. Wenning, a leading expert, says the clearest marker is this: if someone has major autonomic failure-like fainting or bladder control loss-within 3 years of their first tremor or stiffness, it’s almost certainly MSA, not Parkinson’s.What Can Be Done?
There’s no cure. No drug stops MSA from progressing. Treatment is about managing symptoms and keeping people safe as long as possible. For low blood pressure, doctors use fludrocortisone or midodrine. Droxidopa, approved by the FDA in 2014, helps some patients stand without passing out. For bladder issues, medications like oxybutynin or catheterization may be needed. Sleep apnea is treated with CPAP machines. Physical therapy helps maintain mobility longer. Speech therapy prevents choking by teaching safer swallowing techniques. High-dose levodopa is still tried, even though it rarely works. It’s a gamble-but sometimes, even a little improvement matters for quality of life.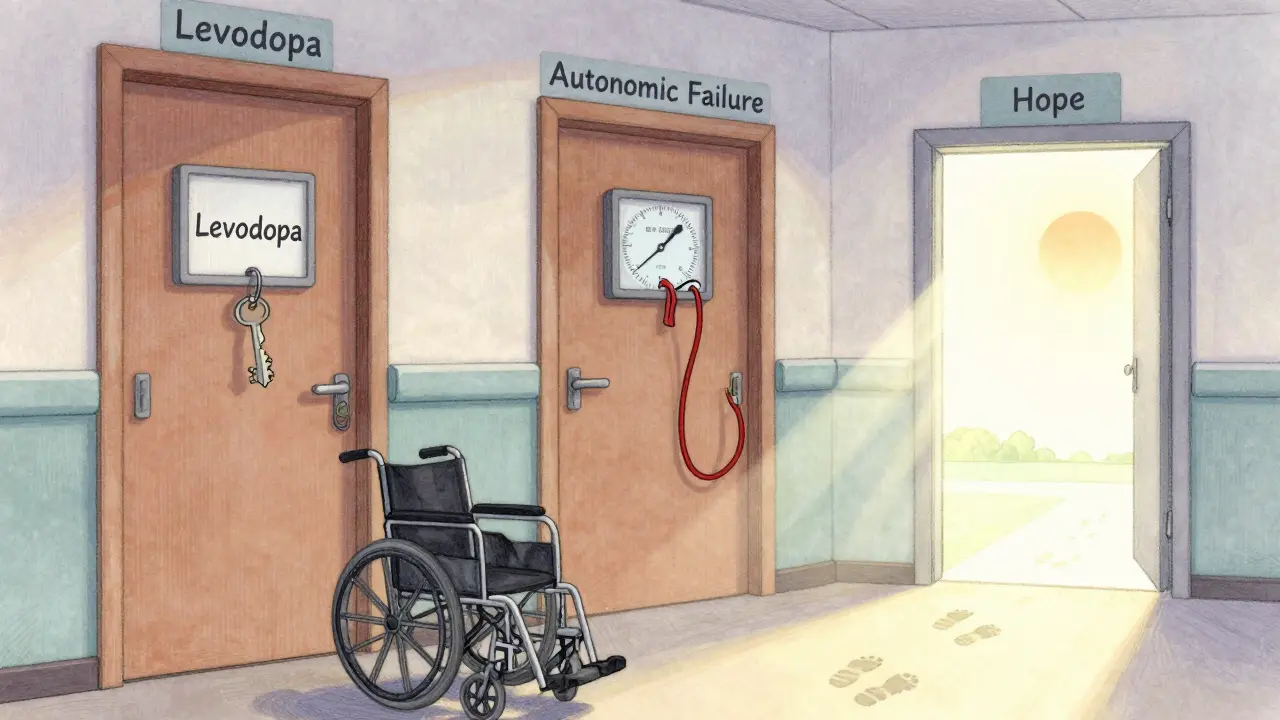
The Future: Hope on the Horizon?
Research is slow. As of late 2023, there are only three active clinical trials worldwide trying to slow or stop MSA. One major study tested a drug targeting alpha-synuclein-the abnormal protein that builds up in MSA brains. The results? Barely any difference compared to placebo. But there’s progress in diagnosis. Scientists are building a biomarker panel: MRI scans of brain volume, blood tests for neurofilament light chain (a protein that spikes when brain cells die), and detailed autonomic tests. If this works, doctors could diagnose MSA within a year of symptoms-before massive damage occurs. Dr. Lucy Norcliffe-Kaufmann puts it plainly: “By the time you see the tremor, half to 70% of the brain cells are already gone.” That’s why early detection is the biggest unmet need.Living With MSA-P: The Human Cost
Real people share stories that statistics can’t capture. One man, diagnosed at 52, said he went from needing a cane to a wheelchair in just four years. Another, 55 and newly diagnosed, wrote: “My doctor said most don’t live past eight years. That’s not a prognosis-it’s a countdown.” A 2021 survey of 327 MSA patients found that 78% rated their quality of life as “poor” or “very poor” within four years of diagnosis. Compare that to Parkinson’s patients at the same stage-only 35% felt that way. MSA doesn’t just take your movement. It takes your independence, your dignity, your sleep, your control over your own body. And it does it fast.Final Thoughts
Multiple System Atrophy isn’t a slow fade. It’s a rapid, relentless decline. Its parkinsonian features mimic Parkinson’s, but the underlying damage is wider, deeper, and deadlier. Autonomic failure is the silent engine of its progression. Survival is measured in years, not decades. Treatment is supportive, not curative. What’s clear is this: if you or someone you know has unexplained dizziness, urinary problems, or voice changes before age 60-and it doesn’t respond to Parkinson’s meds-ask about MSA. Early recognition doesn’t change the outcome yet, but it changes how you live the time you have. Planning for safety, mobility, and comfort matters more than ever.Right now, there’s no miracle. But awareness, early diagnosis, and compassionate care are the only tools we have to make those final years as meaningful as possible.

Sangeeta Isaac
January 20, 2026 AT 18:42Samuel Mendoza
January 22, 2026 AT 09:00Rod Wheatley
January 23, 2026 AT 20:42Malvina Tomja
January 25, 2026 AT 06:40MARILYN ONEILL
January 26, 2026 AT 07:39Stephen Rock
January 27, 2026 AT 19:00Jarrod Flesch
January 28, 2026 AT 06:29shubham rathee
January 29, 2026 AT 12:21Glenda Marínez Granados
January 30, 2026 AT 08:42Melanie Pearson
January 30, 2026 AT 17:32lokesh prasanth
January 31, 2026 AT 12:18Rod Wheatley
January 31, 2026 AT 19:45