Parkinson’s DBS: How Deep Brain Stimulation Works and Who Is a Good Candidate
 Dec, 16 2025
Dec, 16 2025
What Is Deep Brain Stimulation for Parkinson’s?
Deep Brain Stimulation, or DBS, is a surgical treatment for Parkinson’s disease that uses implanted electrodes to send electrical pulses to specific areas of the brain. These pulses help control the abnormal signals causing tremors, stiffness, and slow movement. Unlike medications that change brain chemistry, DBS works like a pacemaker for the brain-regulating activity without drugs.
It’s not a cure. It doesn’t stop Parkinson’s from getting worse. But for the right person, it can cut motor symptoms by 60-80% and reduce the need for levodopa by 30-50%. That means fewer side effects like involuntary movements (dyskinesias) and more predictable days.
Who Really Benefits from DBS?
Not everyone with Parkinson’s is a candidate. The best candidates have had the disease for at least five years and still respond well to levodopa. If your symptoms improve significantly after taking your medication, DBS is likely to help. If your tremors or stiffness don’t get better with levodopa, DBS probably won’t either.
Doctors use the Unified Parkinson’s Disease Rating Scale (UPDRS) to measure this. A 30% or better improvement in motor scores after taking levodopa is the minimum threshold. If you’re barely moving even with medication, DBS won’t fix that.
People with atypical parkinsonism-like progressive supranuclear palsy or multiple system atrophy-rarely benefit. Their symptoms don’t respond to levodopa, and DBS won’t change that. Studies show response rates under 10% in these cases.
What Does the Evaluation Process Look Like?
Getting approved for DBS isn’t just a quick doctor’s visit. It’s a months-long process involving multiple specialists.
- Neurologist evaluation: Confirms you have idiopathic Parkinson’s and not another condition. Tests your levodopa response.
- Neuropsychological testing: Assesses memory, attention, and executive function. If your MMSE score is below 24 or MoCA is below 21, you’re usually not a candidate. DBS can worsen thinking problems in people who already have them.
- 3T MRI scan: Maps your brain in high detail so surgeons know exactly where to place the electrodes.
- Multidisciplinary team review: Neurologist, neurosurgeon, neuropsychologist, and sometimes a speech therapist all review your case together.
This isn’t optional. Skipping steps leads to poor outcomes. One 2022 study found that 30% of patients were disappointed after surgery because their expectations weren’t managed properly. They thought DBS would fix fatigue, depression, or balance issues-things it doesn’t help much with.
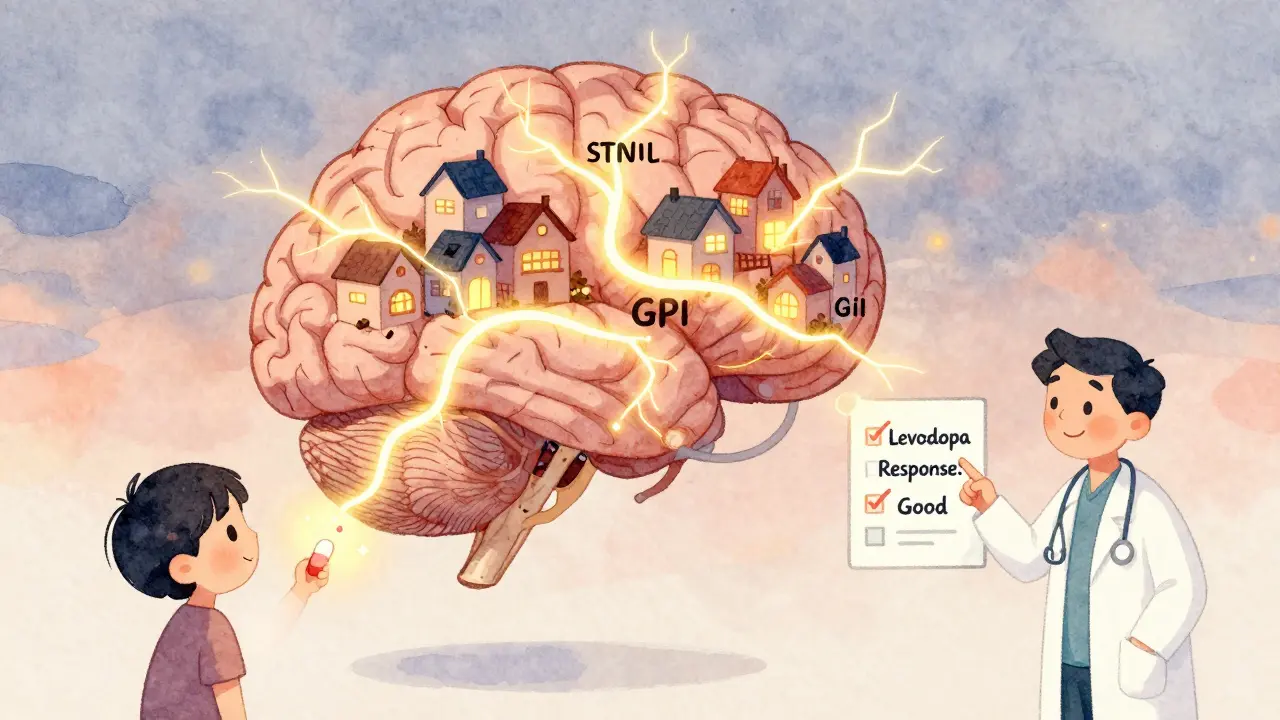
STN vs. GPi: Which Brain Target Is Right for You?
There are two main targets for DBS electrodes in Parkinson’s: the subthalamic nucleus (STN) and the globus pallidus interna (GPi). Both improve movement, but they have different trade-offs.
| Feature | STN (Subthalamic Nucleus) | GPi (Globus Pallidus Interna) |
|---|---|---|
| Medication reduction | High (40-50% less levodopa) | Moderate (10-20% less) |
| Dyskinesia control | Good (46% reduction) | Excellent (70% reduction) |
| Cognitive side effects | Higher risk (word-finding, attention) | Lower risk |
| Best for | Patients wanting to cut meds | Patients with severe dyskinesias or cognitive concerns |
Many patients choose STN because they want to reduce their pill burden. But if you’re already struggling with memory or speech, GPi might be safer. The VA/NINDS CSP #468 trial showed both targets improved motor scores by nearly the same amount-49%-but GPi won on dyskinesia control and brain safety.
What Happens During Surgery?
DBS surgery is done while you’re awake-partly. You’re sedated but responsive so surgeons can test your responses as they place the electrodes. The procedure takes 3 to 6 hours.
First, a metal frame is attached to your head. Then, a 3T MRI guides the team to the target area. Thin electrodes (1.27mm wide) are inserted through small holes in the skull. Microelectrode recording helps confirm they’re in the right spot by listening to brain signals. You might be asked to move your hand or count aloud during this phase.
Once the electrodes are placed, the pulse generator (battery) is implanted under the skin near your collarbone or abdomen. Wires connect the electrodes to the battery under your skin. You’ll wake up with a small bump under your chest.
Most people go home within 24-48 hours. The device isn’t turned on right away-it takes a few weeks for swelling to go down before programming begins.
What Are the Risks?
DBS is safe for most, but it’s not risk-free.
- Surgical risks: 1-3% chance of brain bleed. Less than 1% risk of stroke.
- Hardware issues: 5-15% of patients need a revision. Wires can break, batteries can fail, or leads can shift.
- Infection: 2-5% chance, often within the first year. May require removal of the device.
- Cognitive or mood changes: Some people report trouble finding words, slower thinking, or mild depression. These are often reversible with programming adjustments.
Unlike older procedures like thalamotomy or pallidotomy-which destroy brain tissue permanently-DBS is reversible. If something goes wrong, you can turn it off or remove the hardware.
What About the Cost and Insurance?
DBS costs between $50,000 and $100,000 in the U.S. This includes surgery, hospital stay, device, and follow-ups. Medicare and most private insurers cover it if you meet criteria.
But getting approval can take 3-6 months. Insurers want proof you’ve tried and failed on optimal medication regimens. You’ll need detailed records showing your symptoms and medication history.
Device costs vary by brand. Medtronic’s Percept™ PC and Boston Scientific’s Vercise™ Genus™ are newer systems with rechargeable batteries that last 9-15 years. Older non-rechargeable batteries need replacement every 3-5 years-another surgery.
How Long Does It Take to See Results?
Don’t expect miracles right after surgery. The device is usually turned on 2-4 weeks post-op. Then comes the long process of programming.
It can take 6-12 months to fine-tune the settings. You’ll need monthly visits at first. Each session involves adjusting voltage, frequency, and pulse width while you do tasks like walking, writing, or speaking. Your symptom diary is critical.
Some people feel better within days. Others take months. The EARLYSTIM trial showed quality of life scores improved by 23 points for DBS patients versus 12.5 for those on meds alone-a huge difference.

What Are the Real-Life Experiences?
Real people share mixed stories online.
One user on the Parkinson’s Foundation Forum said: “My OFF time dropped from 6 hours a day to 1 hour. Dyskinesias dropped 90%. But I started forgetting words. Had to do speech therapy.”
Another on Reddit wrote: “My tremors are gone. But planning a meal now takes three times longer. I’m slower to make decisions.”
Those who were disappointed often thought DBS would stop disease progression. It doesn’t. It only treats symptoms that respond to levodopa. Fatigue, balance issues, and speech problems often don’t improve much.
Still, 70-80% of properly selected patients report meaningful improvement. Many say they can return to hobbies, drive again, or live independently longer.
What’s New in DBS Technology?
The field is advancing fast.
Medtronic’s Percept™ PC, approved in 2020, can “listen” to your brain. It records beta wave activity (13-35 Hz), which spikes during Parkinson’s stiffness. This lets the device adjust stimulation automatically. Early results show 27% better symptom control than traditional DBS.
Researchers are now testing DBS in earlier-stage patients. The EARLYSTIM-2 trial is looking at people with only 3 years of Parkinson’s. Early data suggests benefits may be even greater if you intervene sooner.
Future tools might link your Apple Watch to your DBS device, adjusting stimulation when tremors are detected. Genetic testing is also emerging-people with LRRK2 gene mutations respond 15% better to DBS, according to a 2023 Lancet Neurology study.
Why Is DBS So Underused?
Despite its effectiveness, only 1-5% of eligible Parkinson’s patients get DBS. Why?
- Many neurologists don’t refer patients until they’re severely disabled.
- Patients fear brain surgery.
- Insurance delays discourage people.
- Most community hospitals don’t have the team to do it.
Studies show centers doing over 50 DBS procedures a year have 20% fewer complications. If your doctor doesn’t refer you to a high-volume center, ask why.
The Parkinson’s Foundation calls it a “markedly underutilized treatment.” Too many people suffer longer than they need to because they never even got screened.
Final Thoughts: Is DBS Right for You?
DBS isn’t for everyone. But if you’ve had Parkinson’s for five or more years, still respond well to levodopa, and your symptoms are limiting your life, it’s worth exploring.
Don’t wait until you’re stuck in bed or can’t swallow. The best outcomes come from early, thoughtful selection-not desperation.
Ask your neurologist: “Am I a candidate for DBS?” If they say no, ask for a referral to a movement disorders specialist. Don’t settle for “it’s too risky” or “you’re not sick enough.” You deserve to know your options.
Can DBS cure Parkinson’s disease?
No, DBS does not cure Parkinson’s. It doesn’t stop the disease from progressing. It only helps control motor symptoms that respond to levodopa, like tremors, stiffness, and slowness. Non-motor symptoms like fatigue, sleep problems, and memory issues often don’t improve.
How long does a DBS battery last?
Battery life depends on the device. Non-rechargeable batteries last 3-5 years and require replacement surgery. Newer rechargeable systems like Medtronic’s Percept™ PC and Boston Scientific’s Vercise™ Genus™ last 9-15 years. Charging is done at home with a special device, usually once a week.
Is DBS safer than lesioning surgery?
Yes. Lesioning procedures like pallidotomy or thalamotomy destroy brain tissue permanently. If something goes wrong, the damage is irreversible. DBS is adjustable and reversible. You can turn it off or remove the hardware. Complication rates are lower, and outcomes are more predictable.
Can I have an MRI after DBS?
Yes, but only under strict conditions. Most modern DBS devices are MRI-conditional. You need a 3T MRI machine and specific safety protocols. Always inform the radiology team you have a DBS implant. Some older devices still can’t have MRIs at all.
Will I still need to take Parkinson’s meds after DBS?
Most people still need some medication, but usually much less. STN DBS can reduce levodopa doses by 40-50%. GPi DBS typically reduces doses by 10-20%. The goal isn’t to stop meds completely-it’s to reduce side effects like dyskinesias and make daily life more predictable.
How soon can I return to normal activities after surgery?
Most people return to light activities within 2-4 weeks. Driving and heavy lifting are usually avoided for 6 weeks. Full recovery and optimal programming take 6-12 months. Don’t rush the process-fine-tuning the device is just as important as the surgery.
What happens if the device stops working?
If the battery dies or a wire breaks, symptoms will return to their pre-surgery state. It’s not dangerous, but it’s disruptive. Most systems have alerts for low battery. Always keep your programmer device handy and know how to contact your DBS team. Regular check-ups prevent emergencies.

Jane Wei
December 18, 2025 AT 10:38My dad got DBS last year-tremors are basically gone, but now he forgets where he put his keys. Still, he’s driving again and made it to his grandkid’s soccer game. Worth it.
Naomi Lopez
December 19, 2025 AT 04:37Let’s be real-DBS isn’t some miracle cure, it’s a highly engineered neurological hack. The fact that we can now modulate neural circuits with sub-millimeter precision using implanted devices is staggering. And yet, most neurologists still treat it like a last-resort Hail Mary. The real tragedy isn’t the surgery-it’s the systemic delay in referral. If we screened at 3 years instead of 8, we’d see far fewer patients with advanced disability. The EARLYSTIM-2 data is compelling, and yet, inertia reigns.
Martin Spedding
December 20, 2025 AT 20:00STN vs GPi? Bro. Just pick STN. Less meds = less nausea = less crying in the grocery store. GPi? That’s for people who wanna keep their pills and their dementia. Also, why does everyone act like brain surgery is scary? I had a wisdom tooth out that was more traumatic.
Raven C
December 22, 2025 AT 01:17I find it profoundly disturbing that the medical community continues to prioritize motor symptom reduction over the lived experience of non-motor decline. Fatigue, apathy, executive dysfunction-these are the silent killers of quality of life. Yet, we celebrate a 60% tremor reduction as if it’s a victory, while ignoring that the patient now spends 14 hours a day staring at the ceiling, unable to muster the cognitive energy to read a single sentence. This isn’t progress-it’s selective empathy.
Donna Packard
December 23, 2025 AT 06:25My sister was told she wasn’t a candidate because her MMSE was 23. But she’s the same person who organized a community garden and taught herself Spanish. Sometimes the tests don’t capture the whole person. I hope she gets another opinion.
Patrick A. Ck. Trip
December 24, 2025 AT 11:39While I appreciate the comprehensive nature of this overview, I would respectfully suggest that the emphasis on surgical outcomes might inadvertently overshadow the importance of longitudinal psychosocial support. The device may restore motor function, but the emotional recalibration required post-procedure is often underestimated. A multidisciplinary team should include a licensed clinical social worker, not merely a speech therapist.
Jessica Salgado
December 25, 2025 AT 04:26Wait-so if I have LRRK2 mutation, I’m 15% more likely to benefit? That’s wild. I didn’t even know genetic testing was a thing for this. My neuro just said ‘you’re a candidate’ and handed me a pamphlet. No one mentioned genes. I’m gonna ask for a referral to a center that does genetic screening. This changes everything.
Steven Lavoie
December 26, 2025 AT 05:34I’m from Colombia, and here, DBS is practically unheard of outside Bogotá. My cousin’s brother had it done in Chicago-cost him his entire life savings. Insurance didn’t touch it. We need global access, not just elite centers in the U.S. and Europe. This technology shouldn’t be a luxury. It should be a right.