Polypharmacy and Side Effects: How Taking Too Many Medications Increases Health Risks
 Jan, 6 2026
Jan, 6 2026
Polypharmacy Risk Calculator
Enter the number of medications you take daily (including prescription, over-the-counter, vitamins, and supplements) to see your risk level.
Your Risk Assessment
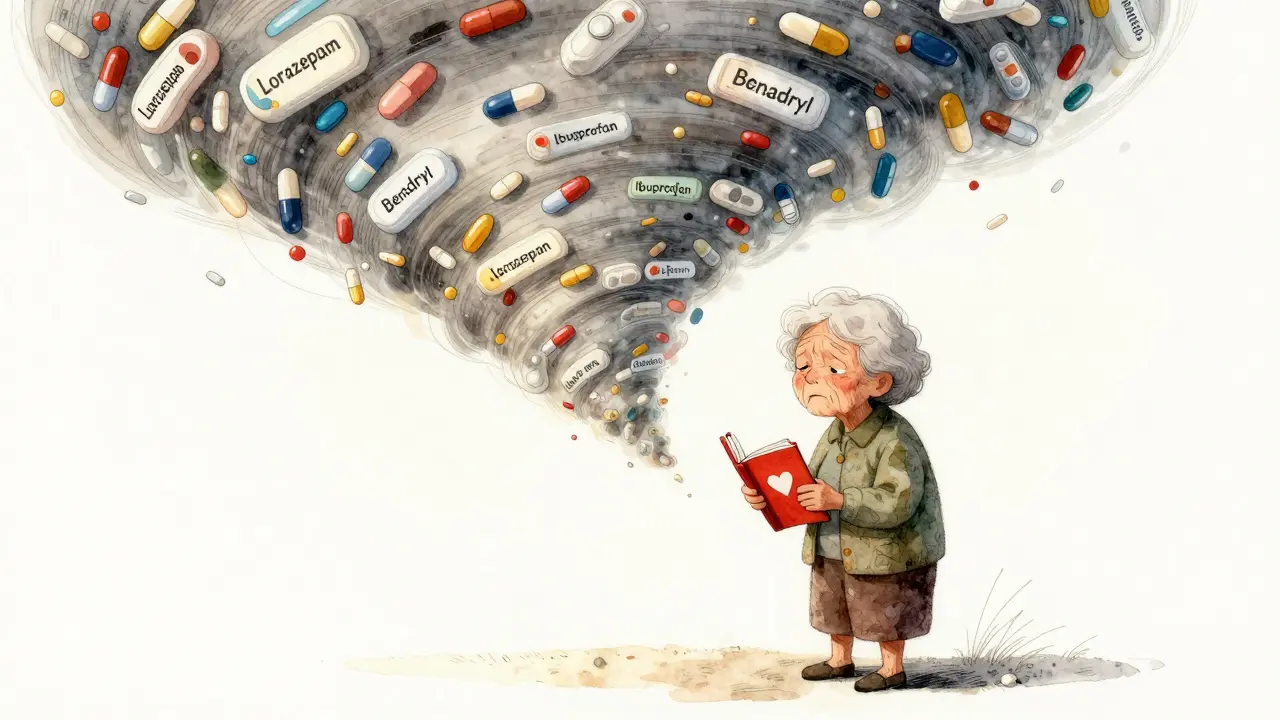
When you’re taking five or more medications every day, it’s not just a routine-it’s a risk. Polypharmacy, the term for using multiple drugs at once, is common among older adults and people with chronic illnesses. But what looks like good medical care can quietly become a danger. The more pills you take, the higher your chance of serious side effects, falls, hospital stays, and even death. This isn’t about overmedication by accident-it’s a growing public health crisis backed by hard data.
What Exactly Is Polypharmacy?
Polypharmacy isn’t just having a few prescriptions. It’s defined as taking five or more medications regularly. That includes prescription drugs, over-the-counter pills, vitamins, and herbal supplements. For someone with heart disease, diabetes, and arthritis, some of these may be necessary. But too often, medications are added without stopping others-leading to a pile-up of drugs that don’t always work together.
The problem isn’t the number alone. It’s whether each drug still makes sense. One person might need five drugs to survive a heart attack. Another might be taking six because a doctor prescribed one for a side effect caused by another. That’s called a medication cascade, and it’s responsible for 30-40% of unnecessary prescriptions in older adults.
How More Medications Mean More Side Effects
Every drug you take changes how your body works. When you add more, those changes don’t just stack-they multiply. Your liver and kidneys, which process medications, slow down with age. That means drugs stay in your system longer, building up to dangerous levels. Even if each drug is safe on its own, together they can cause problems no one expected.
Here’s what happens in real life:
- One medication causes dizziness → a fall → a broken hip → new pain meds → more dizziness → another fall.
- A blood pressure drug causes dry mouth → someone buys an antihistamine for relief → now they’re drowsy and confused.
- Three different drugs affect the same enzyme in your liver → one becomes toxic.
Studies show that people taking five or more medications are 50% more likely to have a dangerous drug interaction. And for those on 10 or more, the risk of a serious side effect jumps to over 80%.
The Real Cost: Falls, Hospitalizations, and Death
Polypharmacy doesn’t just make you feel bad-it puts you in the hospital and kills you.
People on five or more drugs are 1.5 to 2 times more likely to fall. Falls are the leading cause of injury-related death in adults over 65. One study found that 28% more people die each year if they’re taking 10 or more medications compared to those on just one to four.
Hospital stays get longer. On average, polypharmacy patients stay 2 to 19% longer in the hospital than others. Emergency room visits go up by 32%. And the cost? The U.S. spends over $300 billion a year treating problems caused by unnecessary or poorly managed medications.
It’s not just physical. Many patients report feeling overwhelmed. One 72-year-old woman said, “I was taking 17 pills a day and couldn’t remember which ones I’d taken. I felt like a pharmacy on legs.” Another man had to choose between buying his heart medicine or food because his monthly drug bill was $400.
Who’s Most at Risk?
Older adults are the most affected. Nearly 44% of men and 57% of women over 65 take five or more medications. But it’s not just age-it’s the system. Doctors often treat each condition separately, not the whole person. A cardiologist prescribes one drug. A rheumatologist adds another. A neurologist adds a third. No one steps back to see the full picture.
Patients with multiple chronic conditions-like heart failure, diabetes, and kidney disease-are especially vulnerable. But here’s the twist: for some of these patients, multiple medications are life-saving. The key isn’t to stop all drugs-it’s to stop the wrong ones.

What Makes a Medication Inappropriate?
The American Geriatrics Society has a list called the Beers Criteria-a guide to drugs that are risky for older adults. These aren’t banned. But they’re flagged because they cause more harm than good in seniors.
Top offenders include:
- Anticholinergics (like diphenhydramine in Benadryl): cause confusion, memory loss, dry mouth, and constipation.
- Benzodiazepines (like lorazepam or diazepam): increase fall risk and dementia progression.
- NSAIDs (like ibuprofen or naproxen): raise blood pressure, hurt kidneys, and cause stomach bleeding.
These three classes make up 45% of inappropriate prescriptions in older adults. Many are still given because they’re easy to write-“Take one for sleep,” “Take one for pain”-without checking if they’re still needed.
Deprescribing: The Quiet Revolution in Medication Safety
The solution isn’t more drugs. It’s fewer. And it’s called deprescribing.
Deprescribing means carefully stopping medications that aren’t helping-or are hurting. It’s not about going cold turkey. It’s a planned, step-by-step process done with your doctor over weeks or months. You might reduce one drug at a time, watch for changes, and only stop if symptoms don’t get worse.
Studies show that when done right, deprescribing:
- Reduces falls by up to 30%
- Improves mental clarity and energy
- Lowers monthly drug costs by $100-$200
- Decreases hospital visits
One patient on Reddit shared that after stopping three unnecessary pills, her dizziness and confusion vanished. Another said she finally slept through the night after quitting a sleep aid she’d been on for 12 years.
How to Start the Conversation With Your Doctor
If you’re taking five or more medications, ask for a full review. Don’t wait for an annual checkup-request it now.
Here’s what to say:
- “I’m taking [list them all, including vitamins and OTC meds]. Can we go over each one to see what’s still needed?”
- “Which of these is most likely causing side effects like dizziness, fatigue, or confusion?”
- “Is there a drug I can stop safely? What would happen if I did?”
- “Can we try reducing one at a time and see how I feel?”
Bring a list. Write down every pill, capsule, patch, and supplement. Include doses and why you take them. If you don’t know why, say so. That’s the point-you shouldn’t be guessing.

Technology Is Helping-But It’s Not Enough
Tools like MedWise, approved by the FDA in 2022, scan your meds and flag dangerous combinations. Medicare now requires reviews for people on eight or more drugs. But only 12% of medical schools teach polypharmacy. Only 35% of primary care doctors feel confident doing deprescribing.
Technology helps. But the real fix is better communication. A doctor needs to understand your life-not just your labs. Are you skipping doses because it’s too expensive? Are you too tired to manage a 10-pill routine? Are you afraid to ask to stop something?
What You Can Do Today
You don’t need to wait for a system change. Here’s your action plan:
- Make a complete list of every medication and supplement you take. Include doses and reasons.
- Ask your pharmacist to review it. They spot duplicates and interactions doctors miss.
- Set up a medication review with your primary care doctor. Say: “I want to reduce my pill burden.”
- Track side effects in a notebook: dizziness? memory lapses? nausea? fatigue? Write them down.
- Don’t stop anything on your own-but do ask. You have the right to question every prescription.
Every pill you take has a reason. But not every reason still matters. Sometimes, the safest thing you can do is stop taking something.
Why This Matters More Than Ever
By 2030, half of all adults over 65 will be on five or more medications. Without change, adverse drug events will rise 40% and costs will climb $127 billion a year by 2035.
This isn’t just about aging. It’s about how we treat people with complex health needs. We’ve built a system that adds drugs-but rarely removes them. That’s backward.
Health isn’t just about adding treatments. It’s about removing what harms you. The goal isn’t fewer pills for the sake of it. It’s better health, more energy, fewer falls, and more control over your life.
Ask the question. Review your list. Talk to your doctor. You might be surprised what disappears-and what returns when it does.
What is polypharmacy?
Polypharmacy is the regular use of five or more medications at the same time. This includes prescription drugs, over-the-counter medicines, vitamins, and supplements. While some people need multiple drugs for serious conditions, polypharmacy often includes unnecessary or harmful medications that increase side effects and health risks.
Is polypharmacy always dangerous?
No. Polypharmacy can be appropriate when each medication is necessary and carefully chosen-for example, a heart attack survivor taking a beta blocker, statin, aspirin, and ACE inhibitor. The danger comes when medications are added without stopping others, leading to harmful interactions, side effects, or duplications. The issue isn’t the number-it’s whether each drug still serves a clear, safe purpose.
What are the most common side effects of taking too many medications?
Common side effects include dizziness, confusion, memory problems, fatigue, falls, constipation, nausea, and low blood pressure. These are often mistaken for aging-but they’re usually drug-related. Anticholinergics, benzodiazepines, and NSAIDs are the top culprits. One study found that 48% of people on five or more meds experienced side effects they believed were caused by their medications.
How can I reduce my medications safely?
Start by making a complete list of everything you take-including vitamins and OTC drugs. Ask your doctor for a medication review. Don’t stop anything on your own. Instead, ask: “Can we try reducing one drug at a time?” The process, called deprescribing, usually takes 3-6 months. Your doctor will monitor how you feel and adjust slowly. Many patients report better energy, clearer thinking, and fewer falls after reducing unnecessary pills.
Why don’t doctors always check for unnecessary medications?
Many doctors focus on treating one condition at a time-like high blood pressure or arthritis-and don’t look at the full picture. Time limits, lack of training, and pressure to prescribe make it hard to pause and review. Only 35% of primary care doctors feel very confident in deprescribing. But that’s changing. New guidelines and tools like MedWise are helping, but patients need to speak up and ask for a full review.
How much do polypharmacy-related costs add to healthcare?
In the U.S., polypharmacy contributes to over $300 billion in avoidable healthcare costs each year. This includes emergency room visits, hospital stays, long-term care, and treatment of side effects like falls and kidney damage. Patients on 10+ medications spend an average of $5,200 a year on drugs alone-forcing many to skip doses or choose between food and medicine.

Katrina Morris
January 7, 2026 AT 04:33i took 12 pills a day for years and never thought to question them until i started blacking out after dinner
my pharmacist caught 4 duplicates and a benzo i didn't even know i was still on
now i take 5 and actually sleep through the night
Anthony Capunong
January 7, 2026 AT 20:41this is why america is falling apart
people won't take responsibility for their health
they want a pill for everything and then blame the system when they fall down the stairs
grow up
Aparna karwande
January 8, 2026 AT 18:30in india we call this "doctor shopping" - one doctor gives you a pill for blood pressure, another for sugar, another for sleep, another for anxiety, another for constipation from the first four... and no one ever asks if you're actually improving or just medicated into a coma
we need to stop treating symptoms like they're separate wars and start treating the whole human
your body isn't a vending machine
Vince Nairn
January 9, 2026 AT 05:27so let me get this straight... we've built a healthcare system where the only way to get better is to convince your doctor to stop giving you stuff?
brilliant
if this isn't systemic failure i don't know what is
and yes i'm being sarcastic
but also not really
Ayodeji Williams
January 10, 2026 AT 19:43bro i was on 14 pills and my grandma said "son you look like a zombie"
we cut 6 and now i can walk to the store without falling asleep
😭🙏
Kyle King
January 12, 2026 AT 19:39they're not trying to help you
they're trying to keep you dependent
pharma owns the FDA, the doctors, even the pill bottles
they don't want you healthy
they want you buying pills forever
ask yourself why they never teach deprescribing in med school
Kamlesh Chauhan
January 13, 2026 AT 07:49all this talk about pills and nobody mentions the real problem
doctors are overworked and underpaid
they have 7 minutes per patient
they're not evil
they're just drowning
blaming them is lazy
Emma Addison Thomas
January 15, 2026 AT 05:57i had a similar experience with my mother in london
she was on 11 medications after a minor stroke
we worked with her GP over six months to reduce it to four
her balance improved, her mood lifted, and she started gardening again
it wasn't magic
just careful, patient review
Mina Murray
January 15, 2026 AT 12:32you think this is about pills
it's about control
the medical industrial complex needs you sick
they'll give you a pill for your sadness then another for the constipation from the first pill then another for the anxiety from the second
and then they'll charge you $800 for a blood test to prove you're still broken
you're not a patient
you're a revenue stream
Christine Joy Chicano
January 16, 2026 AT 18:24the most terrifying part isn't the drug interactions
it's how often people don't even know what they're taking
i met a woman who was taking a sleep aid she'd been prescribed in 2009
she didn't remember why
her doctor didn't know she was still on it
and she'd been taking it every night for 15 years
that's not medicine
that's a ghost in the machine
Jonathan Larson
January 17, 2026 AT 20:27the ethical framework of modern medicine has become inverted
we prioritize intervention over observation, prescription over reflection, and accumulation over reduction
the Hippocratic oath speaks first of "do no harm"-yet our systems incentivize the opposite
deprescribing is not merely clinical practice
it is an act of moral courage
and the patient, armed with a list and a question, becomes the most vital agent of healing
the system may be broken
but the humanity within it remains intact
if we choose to honor it