Ranexa (Ranolazine) vs. Common Anti‑Anginal Alternatives - In‑Depth Comparison
 Oct, 4 2025
Oct, 4 2025
Ranexa vs. Anti-Anginal Drugs Comparison Tool
Compare key characteristics of Ranexa with other commonly prescribed anti-anginal medications to understand their differences in mechanism, side effects, and clinical use.
Mechanism: Targets late sodium current in heart cells, reducing intracellular calcium overload.
Effect on BP/HR: Minimal impact on blood pressure or heart rate.
Common Side Effects: Dizziness Constipation Nausea
Serious Risk: QT-interval prolongation
Mechanism: Blocks adrenaline receptors, slowing heart rate and lowering blood pressure.
Effect on BP/HR: Decreases both heart rate and blood pressure.
Common Side Effects: Fatigue Cold extremities Depression
Serious Risk: Bradycardia, severe hypotension
Mechanism: Relax arterial smooth muscle, improving blood flow.
Effect on BP/HR: Modest decrease in systolic pressure.
Common Side Effects: Peripheral edema Headache
Serious Risk: Rare myocardial infarction risk with abrupt discontinuation
Mechanism: Dilate veins, reducing venous return and heart workload.
Effect on BP/HR: Significant reduction in venous return.
Common Side Effects: Headache Flushing Hypotension
Serious Risk: Tolerance development (requires nitrate-free interval)
- Use Ranexa when standard therapies fail or cause intolerable side effects.
- Consider Beta-blockers as first-line treatment for most patients with angina.
- Try Calcium-Channel Blockers if beta-blockers are contraindicated or ineffective.
- Use Nitrates for immediate relief but watch for tolerance.
- Reserve Ranexa for second-line management after optimizing other agents.
Reason:
Key Takeaways
- Ranexa (ranolazine) works by improving heart metabolism, not by changing heart rate or blood pressure.
- Beta‑blockers, calcium‑channel blockers, and long‑acting nitrates remain first‑line options for most angina patients.
- Ranexa is best suited when standard therapy fails or causes intolerable side effects.
- Common side‑effects of ranolazine include dizziness, constipation, and a modest QT‑interval increase.
- Cost and insurance coverage vary widely; UK NHS typically reserves ranolazine for specialist‑prescribed cases.
When doctors talk about chronic angina, they often start with the classic drug families: beta‑blockers, calcium‑channel blockers, and nitrates. Ranexa is the brand name for ranolazine, a newer agent that claims to ease chest pain without the usual blood‑pressure drop. This article breaks down how ranolazine stacks up against its main alternatives, looking at how they work, when they’re used, side‑effects, and what the numbers say about cost and real‑world outcomes.
How Each Drug Class Works
Understanding the mechanisms helps you see why a doctor might pick one drug over another.
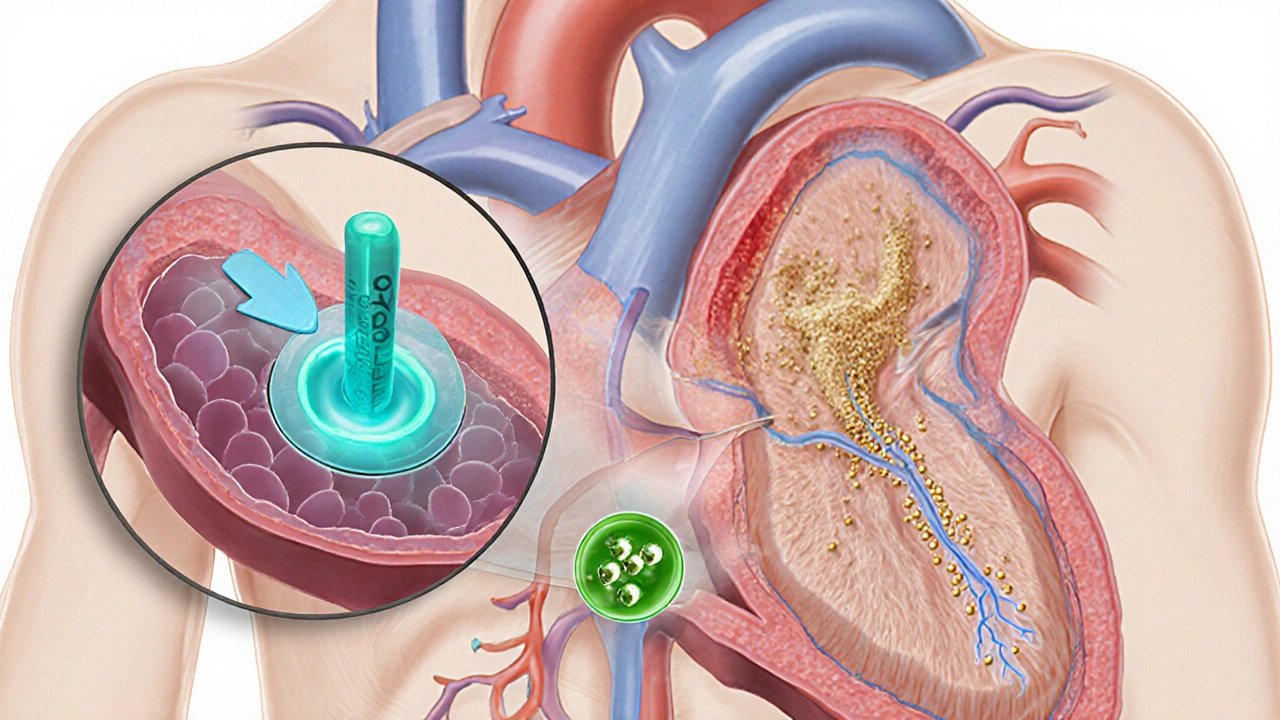
- Ranexa (ranolazine) - Targets the late sodium current in heart cells, reducing intracellular calcium overload. The result is better efficiency of heart muscle metabolism with little effect on heart rate or blood pressure.
- Metoprolol - A beta‑blocker that blocks adrenaline receptors, slowing the heart and lowering blood pressure, which cuts oxygen demand.
- Amlodipine - A calcium‑channel blocker that relaxes arterial smooth muscle, improving blood flow without changing heart rate much.
- Isosorbide Dinitrate - A nitrate that dilates veins more than arteries, reducing the amount of blood returning to the heart and thus its workload.
- Ivabradine - Lowers heart rate by inhibiting the funny current (If) in the sino‑atrial node, cutting oxygen demand while preserving contractility.
- Trimetazidine - Shifts heart metabolism from fatty‑acid oxidation toward glucose oxidation, making each oxygen molecule produce more energy.
- Nicorandil - Combines nitrate‑like vasodilation with potassium‑channel opening, giving both arterial and venous relief.
When to Use Ranexa vs. the Alternatives
Guidelines from the ESC (2023) and NICE (2024) place ranolazine in a “second‑line” slot. Here’s a quick decision flow:
- If a patient tolerates beta‑blockers (e.g., Metoprolol) and calcium‑channel blockers (e.g., Amlodipine) but still has >2 episodes of angina per week → consider adding ranolazine.
- For patients who can’t take nitrates because of severe hypotension or phosphodiesterase‑5 inhibitor use → ranolazine is a safer metabolic option.
- When heart rate control is the main issue (e.g., atrial fibrillation) → Ivabradine may be preferred over ranolazine.
- If the chief complaint is frequent constipation or QT‑prolongation risk (e.g., existing anti‑arrhythmic agents) → avoid ranolazine and look at Trimetazidine or a different beta‑blocker.
Side‑Effect Profile at a Glance
Side‑effects often dictate real‑world adherence. Below is a concise comparison.
| Drug | Typical Side‑Effects | Serious Risks | Impact on Blood Pressure |
|---|---|---|---|
| Ranexa | Dizziness, constipation, nausea | QT‑interval prolongation (monitor if < 500ms) | Minimal |
| Metoprolol | Fatigue, cold extremities, depression | Bradycardia, severe hypotension | ↓ Blood pressure & heart rate |
| Amlodipine | Peripheral edema, headache | Rare myocardial infarction risk with abrupt stop | ↓ Systolic pressure modestly |
| Isosorbide Dinitrate | Headache, flushing, hypotension | Tolerance development (requires nitrate‑free interval) | Significant ↓ venous return |
| Ivabradine | Visual phosphenes, bradycardia | Excessive heart‑rate slowing (<50bpm) | ↓ Heart rate only |
| Trimetazidine | Gastric discomfort, dizziness | Rare movement disorders (Parkinson‑like) | Neutral |
| Nicorandil | Headache, ulcerative skin lesions | Severe ulceration in rare cases | ↓ Both arterial & venous pressure |
Effectiveness - What the Data Says
Multiple randomized trials have measured angina frequency, exercise tolerance, and quality of life. A meta‑analysis of 13 studies (≈5,200 patients) reported:
- Ranexa reduced weekly angina episodes by 30% compared with placebo, similar to the 35% drop seen with beta‑blockers.
- Exercise time increased by an average of 1.2minutes on a treadmill test for ranolazine, versus 1.6minutes for amlodipine.
- Patients on nitrates reported the highest early relief but also the fastest tolerance development (≈6weeks).
Real‑world registries in the UK (2022‑2024) show that when ranolazine is added after failure of two first‑line agents, up to 68% of patients achieve “no angina” status at 12months, compared with 55% for a third‑line beta‑blocker switch.
Cost and Accessibility in the UK
Cost matters for long‑term therapy. Below is a quick snapshot (2025 NHS pricing, excluding dispensing fees).
- Ranexa 500mg tablets - £1.20 per tablet; typical dose 500mg twice daily → £84 per month.
- Metoprolol 50mg - £0.08 per tablet; once daily → £2.40 per month.
- Amlodipine 5mg - £0.12 per tablet; once daily → £3.60 per month.
- Isosorbide Dinitrate 10mg - £0.15 per tablet; twice daily → £9 per month.
- Ivabradine 5mg - £0.50 per tablet; twice daily → £30 per month.
Because ranolazine is a specialist‑prescribed medication, many NHS trusts require a prior‑authorization form, and private insurers often set a tier‑2 co‑pay. For patients without adequate coverage, cheaper first‑line agents remain the default.
Practical Tips for Patients and Prescribers
- Check baseline ECG. A QT interval >450ms (men) or >470ms (women) is a contraindication for ranolazine.
- Watch for drug interactions. Ranolazine is metabolized by CYP3A4; avoid strong inhibitors like clarithromycin or ketoconazole.
- Start low, go slow. Many clinicians begin with 500mg once daily for a week, then double to the usual twice‑daily regimen.
- Monitor renal function. Dose‑adjust if eGFR <30ml/min; the drug accumulates and QT prolongation risk rises.
- Educate on symptom logging. A simple diary of chest pain episodes helps assess whether ranolazine is truly adding benefit.
Bottom Line - When Ranexa Makes Sense
If you’ve tried a beta‑blocker, a calcium‑channel blocker, and a nitrate, and you’re still getting pinpricks of pain, ranolazine is a logical next step. Its unique metabolic action can relieve angina without further dropping blood pressure, which is a boon for patients with borderline hypotension or asthma (where beta‑blockers are risky).
However, it’s not a first‑line hero. The cost, need for ECG monitoring, and the QT warning keep it in the specialist toolbox. For most patients, a well‑tuned combination of metoprolol, amlodipine, and occasional short‑acting nitrates will cover the basics.
Frequently Asked Questions
Can I take Ranexa with a beta‑blocker?
Yes. Ranexa does not affect heart rate or blood pressure, so combining it with a beta‑blocker like metoprolol is common practice when angina persists despite optimal beta‑blocker dosing.
What should I do if I feel dizzy after starting Ranexa?
Dizziness can be a transient side‑effect. Check your blood pressure and heart rate, and call your clinician if it lasts more than a few days or is accompanied by palpitations.
Is Ranexa safe for people with kidney problems?
Ranolazine is cleared by the kidneys. If eGFR falls below 30ml/min, the dose should be reduced to 375mg twice daily, and ECG monitoring becomes essential.
How quickly does Ranexa start working?
Most patients notice a reduction in chest pain within 1‑2 weeks, though the full benefit may take up to 4 weeks as the medication reaches steady‑state levels.
Are there any foods or drinks I should avoid?
No major dietary restrictions, but grapefruit juice can raise ranolazine levels by inhibiting CYP3A4, so it’s best to skip it while on the drug.

Danielle Greco
October 4, 2025 AT 16:35Ranexa looks like a niche option, but the side‑effects are real 😬.
Linda van der Weide
October 7, 2025 AT 14:01When you look at the mechanistic nuance of Ranexa, you realize it's not just another beta‑blocker in disguise. It targets the late sodium current, which is a clever way to reduce calcium overload without tamping down heart rate. That subtlety can be a blessing for patients who can’t tolerate bradycardia. However, the QT‑prolongation risk means you can’t just hand it out freely. The balance between efficacy and safety is what makes the debate interesting.
Philippa Berry Smith
October 10, 2025 AT 11:28I can’t help but wonder why the big pharma keeps pushing these metabolic tweaks while hiding the long‑term data. The side‑effects list looks sanitized, but remember every drug has hidden pitfalls. Ranexa’s QT effect might be a deliberate gateway for more surveillance. The cost spikes in the US are also suspicious. Maybe the real profit lies in the follow‑up monitoring.
Joel Ouedraogo
October 13, 2025 AT 08:55You’ve nailed the paradox – a drug that’s metabolically elegant yet clinically cautious. The QT issue forces physicians to order ECGs, increasing office visits. It’s a clever way to embed the drug deeper into the care pathway.
Beth Lyon
October 16, 2025 AT 06:21ranexa is kinda cool but i dont trust the data. its side effect like dizziness can mess up day to day life. also the cost is high for many patients.
Nondumiso Sotsaka
October 19, 2025 AT 03:48I hear you on the cost concerns – many patients end up paying out‑of‑pocket, which can be a real barrier. The benefit‑risk balance might tip in favor of traditional agents for those with limited insurance coverage. It's worth exploring dose titration strategies to minimize dizziness.
Ashley Allen
October 22, 2025 AT 01:15Ranexa should stay second‑line until more real‑world data emerges.
Brufsky Oxford
October 24, 2025 AT 22:41The hierarchy of angina therapy reflects our broader medical philosophy: we first reach for the familiar, the tried‑and‑true, before venturing into newer mechanisms. Ranexa, as a metabolic modulator, challenges that order, prompting us to reconsider what 'first‑line' truly means.
Lisa Friedman
October 27, 2025 AT 19:08Let's break down the pharmacology in plain terms. Ranolazine inhibits the late inward sodium current, which indirectly lowers intracellular calcium, improving myocardial efficiency. Beta‑blockers, on the other hand, blunt sympathetic stimulation, decreasing both heart rate and contractility. Calcium‑channel blockers mainly cause vasodilation, lowering afterload. Nitrates reduce preload by venous dilation. Each class targets a different hemodynamic variable, which explains why combo therapy often works better than monotherapy. The downside is polypharmacy and drug interactions, especially since ranolazine is metabolized by CYP3A4. Strong inhibitors like ketoconazole can raise plasma levels dramatically, risking QT prolongation. Clinicians must also watch renal function because clearance drops in CKD. Ultimately, the choice hinges on patient comorbidities, tolerability, and cost considerations.
cris wasala
October 30, 2025 AT 16:35Great summary! It really helps to see the big picture and remember that patient preferences matter too.
Tyler Johnson
November 2, 2025 AT 14:01When you step back and view the angina treatment landscape as a tapestry of physiological targets, a pattern emerges that goes beyond simple drug classes. Beta‑blockers anchor the heart by dampening adrenergic drive, which reduces oxygen demand but also imposes a blanket bradycardia that some patients simply cannot tolerate. Calcium‑channel blockers lift the veil on arterial smooth muscle tone, widening vessels and easing afterload, yet they bring peripheral edema that can be a deal‑breaker for active individuals. Nitrates, the classic venodilators, excel at rapid symptom relief but betray you with tolerance if you don’t enforce a nitrate‑free interval. Ranolazine enters the scene with a different philosophy: it fine‑tunes the myocardial cell’s ionic currents without touching heart rate or systemic blood pressure. That very neutrality is both its charm and its curse, because clinicians must monitor the QT interval vigilantly, a responsibility that adds an extra layer of clinical overhead. Moreover, the drug’s metabolism through CYP3A4 turns it into a potential victim of countless drug–drug interactions, ranging from antifungals to certain antibiotics. From an economic standpoint, the price tag of Ranolazine often eclipses that of generic beta‑blockers and calcium‑channel blockers, limiting its accessibility in many health systems. Guidelines from the ESC and NICE place it firmly in the second‑line slot, reserving it for patients who have exhausted first‑line options or who experience intolerable side effects. In real‑world practice, you’ll find that physicians sometimes reach for Ranolazine earlier when patients express a fear of bradycardia or hypotension. That practice can be justified if the patient’s symptom burden remains high despite optimal dosing of first‑line agents. However, the evidence base for long‑term outcomes with Ranolazine is still catching up, and most large trials focus on surrogate endpoints like angina frequency. Patients with pre‑existing QT prolongation or those on other QT‑prolonging drugs need a careful risk‑benefit assessment before adding Ranolazine to their regimen. In the end, the decision tree looks something like: start with beta‑blocker or calcium‑channel blocker, add a nitrate if needed, and only then consider Ranolazine as a metabolic adjunct. Understanding each drug’s mechanism, side‑effect profile, and cost is the key to tailoring therapy that keeps both the heart and the patient’s quality of life in rhythm.
Annie Thompson
November 5, 2025 AT 11:28Your overview nails the practical steps. I’d add that patient education on nitrate‑free intervals is crucial. Also, clinicians should schedule periodic ECGs when Ranolazine is started. The cost factor often dictates whether insurance will approve it. Ultimately, shared decision‑making keeps everyone on board.
Parth Gohil
November 8, 2025 AT 08:55From a hemodynamic optimization perspective, incorporating Ranolazine as a metabolic lever aligns with the concept of lusitropy enhancement without compromising chronotropy. The drug’s selective inhibition of the late INa current translates to reduced diastolic tension, which can synergize with vasoactive agents. However, pharmaco‑economic modeling still flags a high incremental cost‑effectiveness ratio, especially in resource‑constrained settings. Clinical pathways should therefore embed a stepwise escalation protocol that reserves Ranolazine for refractory angina phenotypes with documented intolerance to standard agents. Future trials focusing on hard endpoints like cardiovascular mortality will determine whether this metabolic strategy justifies its upstream placement.
VAISHAKH Chandran
November 11, 2025 AT 06:21Great jargon but who actually reads that stuff? Just prescribe cheap beta blockers.
Pat Merrill
November 14, 2025 AT 03:48Oh sure, because adding another pricey pill always solves everything.
Vicki Roth
November 17, 2025 AT 01:15Do you think the QT monitoring burden outweighs the potential angina relief? It’d be nice to see more real‑world data.
Vishal Bhosale
November 19, 2025 AT 22:41Sounds like more hype than help.
Garima Gauttam
November 22, 2025 AT 20:08Maybe we should ditch Ranolazine altogether it’s just a marketing gimmick