Rifampin and Birth Control: What You Need to Know About Contraceptive Failure Risks
 Dec, 12 2025
Dec, 12 2025
Rifampin Backup Contraception Calculator
This calculator determines the safe date to stop backup contraception after finishing rifampin treatment. Based on CDC and ACOG guidelines, you must use backup contraception for 28 days after your last rifampin dose due to enzyme induction in the liver.
You can stop backup contraception on:
Always consult your healthcare provider before stopping backup methods. This tool follows CDC guidelines for rifampin users.
When you're taking rifampin for tuberculosis or a stubborn staph infection, the last thing you should be worrying about is whether your birth control is still working. But here’s the hard truth: rifampin can make hormonal birth control useless - and it’s one of the only antibiotics that does this reliably.
Why Rifampin Breaks Birth Control
Rifampin doesn’t just kill bacteria. It also tricks your liver into working overtime. It turns on enzymes - specifically CYP3A4 - that break down hormones faster than normal. That includes the estrogen and progestin in your pill, patch, or ring. When those hormones get metabolized too quickly, your body never reaches the level needed to stop ovulation. Studies show rifampin can slash ethinyl estradiol levels by up to 67% and progestin levels by over 50%. That’s not a small drop. That’s enough to let ovulation happen. And once you ovulate, pregnancy becomes possible - even if you’ve been taking your pill perfectly. This isn’t theoretical. Since the 1970s, there have been real cases of women getting pregnant while on rifampin and birth control together. The mechanism is clear, the data is consistent, and the risk is real.It’s Not Just the Pill
Many people think this only applies to oral contraceptives. It doesn’t. Any hormonal birth control that relies on estrogen or progestin is at risk:- Combined pills (estrogen + progestin)
- Progestin-only pills (mini-pills)
- The patch (Ortho Evra)
- The ring (NuvaRing)
- Hormonal IUDs (Mirena, Kyleena, etc.) - though evidence is mixed
What About Other Antibiotics?
You’ve probably heard warnings about antibiotics and birth control. Maybe your doctor told you to use condoms while on amoxicillin or azithromycin. But here’s the thing: for almost every other antibiotic, that advice is outdated. Penicillin, tetracycline, erythromycin, azithromycin - none of these have been proven to reduce contraceptive effectiveness in controlled studies. There were a few scattered reports of pregnancy in the 1970s and 80s, but those were likely coincidences. No consistent pattern emerged. No pharmacokinetic changes were found. No increase in ovulation. Rifampin is the exception. It’s the only antibiotic with strong, reproducible evidence of causing contraceptive failure. The American College of Obstetricians and Gynecologists, the CDC, and the WHO all agree: only rifampin (and its cousin rifabutin) require backup contraception.Rifabutin: The Lesser Known Risk
If you’re being treated for HIV-related infections like MAC (Mycobacterium avium complex), you might be prescribed rifabutin instead of rifampin. It’s similar, but weaker. Still, it’s not safe. Rifabutin reduces hormone levels by about 20-30% - less than rifampin, but enough to be dangerous. The CDC still recommends backup contraception if you’re on rifabutin and hormonal birth control. Don’t assume it’s fine just because the dose is lower.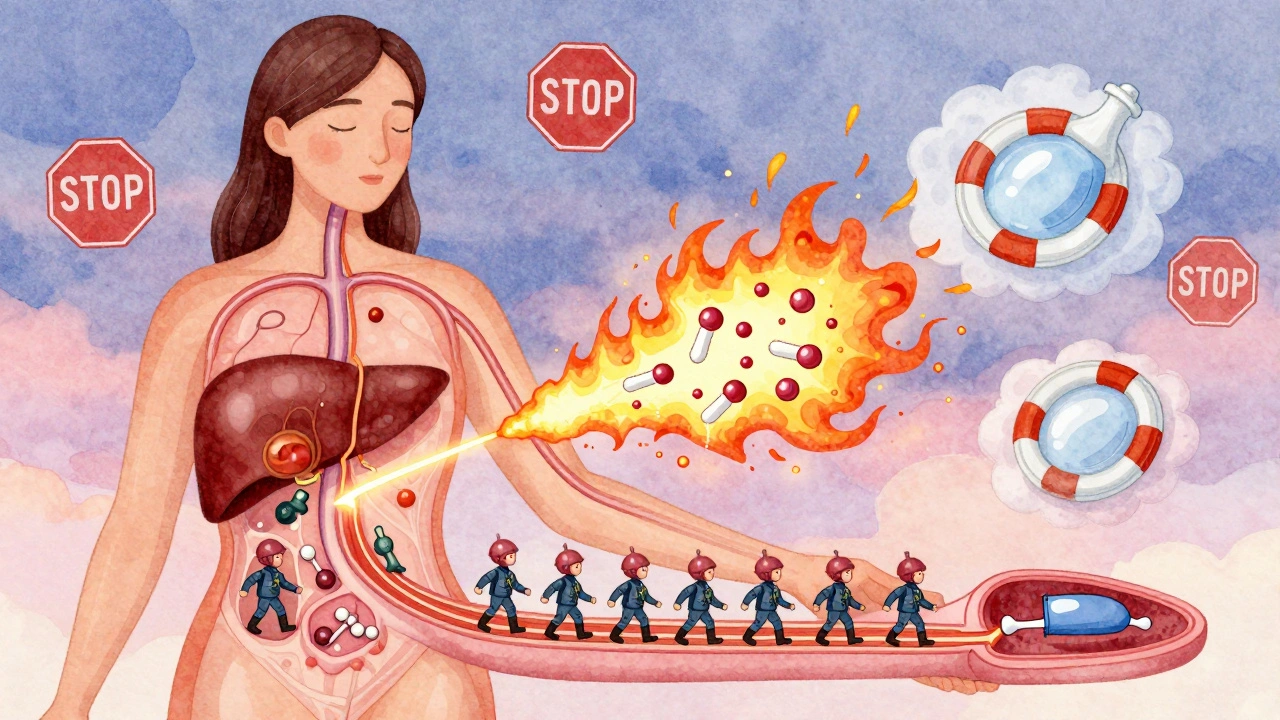
How Long Does the Risk Last?
This is where most people get it wrong. Rifampin’s half-life is only 3-4 hours. So you might think once you stop taking it, the risk is gone. It’s not. The enzyme induction lasts weeks. Your liver keeps producing those extra enzymes for 2-4 weeks after your last dose. That means your birth control stays ineffective long after you finish the antibiotic. The CDC and ACOG both say: use backup contraception - like condoms or a copper IUD - for the entire time you’re on rifampin and for 28 days after you stop. Skip that 28-day window, and you’re rolling the dice.What Should You Do?
If you’re prescribed rifampin and use hormonal birth control, here’s what to do right now:- Stop relying on your pill, patch, or ring as your only method.
- Switch to a non-hormonal backup: copper IUD or condoms (used correctly every time).
- Don’t wait for your doctor to bring it up - ask if you’re not told.
- Keep using backup contraception for 28 days after your last rifampin dose.
- If you’re on a long-term TB regimen, consider switching to a non-hormonal method permanently.
Why Don’t More Doctors Know This?
A 2017 survey found only 42% of primary care doctors consistently warn patients about this interaction. Twenty-eight percent still tell patients to use condoms with all antibiotics. That’s not just wrong - it’s dangerous. It trains people to ignore warnings. Meanwhile, a 2022 study showed 63% of women on rifampin received no proper counseling about birth control. That’s unacceptable. This isn’t a rare edge case. It’s a well-documented, high-stakes interaction that affects thousands of women every year.

Sheldon Bird
December 13, 2025 AT 20:52Yikes, I had no idea rifampin did this. I was on it for a bad staph infection last year and just kept taking my pill like normal. 😅 Glad I didn’t get pregnant, but I’m definitely switching to condoms now. Thanks for the heads-up!
John Fred
December 14, 2025 AT 23:21Bro, this is CYP3A4 induction 101. Rifampin is a potent nuclear-grade enzyme inducer - it’s like your liver goes full turbo mode and metabolizes every estrogen molecule like it’s last call at a bar. 🚨 Progestin? Gone. Pill? Useless. Patch? Trash. Ring? Fuggedaboutit. Only copper IUDs and condoms are safe. No cap. CDC says so. ACOG says so. Your doctor probably doesn’t, but they should. 📉
Hamza Laassili
December 16, 2025 AT 21:28OMG WHY DO DOCTORS KEEP LYING TO WOMEN?!?!?! I read this and my blood boiled. My cousin got pregnant on rifampin and they told her it was 'just bad luck'... NO. IT WAS MEDICAL NEGLIGENCE. WHY ISN'T THIS ON EVERY RX LABEL?!?!?!!!
Rawlson King
December 17, 2025 AT 12:53Let me be blunt: if you’re relying on hormonal birth control while on rifampin, you’re not being responsible-you’re being reckless. This isn’t a 'maybe' or a 'might.' It’s a biochemical certainty. You wouldn’t drive drunk. Don’t have unprotected sex while on this drug. Period.
Cole Newman
December 17, 2025 AT 22:47Wait, so you’re saying the patch and ring are just as bad as the pill? I thought those were 'better' because they're steady-state. But you’re telling me the liver doesn’t care how it gets the hormones? That’s wild. So even if you’re on a low-dose pill, you’re still screwed? 😳
Casey Mellish
December 19, 2025 AT 20:00As an Aussie who’s seen too many patients misunderstand this, I can confirm: this interaction is criminally under-discussed. We’ve got a national health system here, and even our GPs miss it. The copper IUD is the MVP. It’s the only thing that doesn’t care what your liver is doing. Also, 28 days post-rifampin? Non-negotiable. Your liver doesn’t reset on a schedule you like.
Tyrone Marshall
December 21, 2025 AT 10:50There’s something deeply human here - we trust our bodies to respond predictably. But biology doesn’t care about our assumptions. Rifampin doesn’t attack birth control - it rewires your metabolism. And that’s terrifying. We think medicine is about fixing things, but sometimes it’s about reminding us how fragile control really is. The copper IUD isn’t just a device - it’s a quiet act of reclaiming autonomy.
Emily Haworth
December 23, 2025 AT 01:07Okay but… what if your doctor is just lazy? I think big pharma doesn’t want you to know this because copper IUDs are cheap and they make billions off pills. And now I’m paranoid about EVERYTHING. 😵💫 My OB said ‘it’s fine’ but now I’m wondering if she even read the study. What if my Mirena is useless too? I’m gonna sleep with a flashlight and a condom in my pocket now.
Himmat Singh
December 23, 2025 AT 18:27It is imperative to note, with the utmost precision, that the pharmacokinetic interaction between rifampin and hormonal contraceptives is not merely an anecdotal phenomenon but a well-documented, peer-reviewed, and statistically significant metabolic alteration mediated by hepatic cytochrome P450 enzyme induction. One must not conflate this with the negligible interactions observed with non-inducing antibiotics. The clinical imperative is unambiguous.
Lara Tobin
December 24, 2025 AT 22:41I’m so glad someone finally wrote this. I was terrified after I got pregnant on rifampin and didn’t know if it was my fault. No one warned me. I felt so alone. Thank you for saying this so clearly. I hope other women don’t have to go through that.
Scott Butler
December 25, 2025 AT 12:02Why are we even using hormonal birth control anymore? It’s all a scam. Just get sterilized if you don’t want kids. This whole system is designed to keep women dependent on pills that get ruined by one antibiotic. Pathetic.
Deborah Andrich
December 25, 2025 AT 19:50This post saved my life. I was on rifampin for TB and thought my IUD was enough. I didn’t know the enzymes kept working after I stopped. I switched to a copper IUD the next day. No more panic. No more guesswork. Just safety. Thank you.
Michael Gardner
December 26, 2025 AT 02:27Actually, the 2023 Nexplanon study had only 47 women. That’s not enough to say it’s safe. And the CDC hasn’t changed their guidance. So no, don’t assume implants are magic. You’re still playing Russian roulette if you skip condoms.