Shin Splints vs Stress Fractures: Evidence-Based Return-to-Run Plans
 Feb, 7 2026
Feb, 7 2026
Running hurts. Not the good kind of hurt - the kind that means you’re pushing your limits. This is the shin splints kind. The sharp, burning pain along the inside of your shin that starts after 10 minutes and doesn’t go away. Or worse - the deep, aching throb that tells you something inside your bone is breaking down. You’ve been told to rest. But what does that really mean? How long? When can you run again? And why do some runners bounce back in weeks while others relapse again and again?
The truth is, shin splints and stress fractures aren’t the same injury. They’re often lumped together, but they need completely different approaches. Mixing them up is why so many runners end up right back where they started - or worse.
Shin Splints vs Stress Fractures: Know the Difference
Shin splints - or medial tibial stress syndrome (MTSS) - is inflammation of the muscles, tendons, and bone tissue around your tibia. It’s common. About 1 in 5 running injuries is MTSS. Pain is usually diffuse, feels like a dull ache along the inner edge of the shin, and gets better as you warm up. It’s often linked to overtraining, poor footwear, or weak hips.
Stress fractures - or bone stress injuries (BSIs) - are tiny cracks in the bone. They’re more serious. Up to 16% of running injuries are BSIs, and women are at higher risk. Pain is sharp, localized, and gets worse with activity. Press on the spot - if it hurts like a bruise, that’s a red flag. You can’t just ‘run through it.’ Bone doesn’t heal under load. If you keep running, a small crack becomes a full fracture.
Here’s the kicker: MRI scans show that 40% of runners diagnosed with shin splints actually have early-stage stress fractures. That’s why guessing doesn’t work. If pain lasts more than 7 days despite rest, get imaging.
Phase 1: Stop. Rest. Assess.
First rule? Stop running. Not ‘take a few days off.’ Not ‘switch to cycling.’ Stop. Full stop.
For MTSS, you need 3-10 days of non-weight-bearing activity until you can walk pain-free. For stress fractures? You’re looking at 4-6 weeks minimum before even thinking about loading. Bone remodeling cycles take 90-120 days. Rushing this stage is why recurrence rates hit 19-32%.
During this time, cross-train. Pool running is ideal - it mimics running motion with zero impact. Cycling, elliptical, and rowing are fine too. Keep your heart strong. Your legs don’t need to run to stay fit.
Don’t skip the assessment. Recurrent stress fractures? Get a DXA scan. One in four female runners with repeat injuries have low bone density. And 31% of them have RED-S - Relative Energy Deficiency in Sport. That’s when your body doesn’t have enough fuel to repair itself. No amount of stretching or foam rolling fixes that. You need calories, protein, and sleep.
Phase 2: Rebuild Strength - No Running Yet
Once you can walk without pain, it’s time to rebuild what got you here. Weak calves? Poor hip control? That’s your root cause.
Start with double-leg heel raises. Do 3 sets of 15-20 reps, twice a day. No pain. If you feel discomfort over 2/10, stop. This isn’t a workout - it’s therapy. Progress to single-leg raises only after you can do 20 reps pain-free for a week.
Then add step-ups. Stand on a 4-6 inch step, lift one leg, and slowly lower your heel. Do 3 sets of 10-15 per leg. This strengthens your calf and tibialis posterior - the muscle that supports the arch and absorbs shock.
And don’t forget your hips. Gluteus medius weakness is present in 57% of runners who re-injure. Do clamshells, side leg lifts, and banded walks. 3 sets of 15 reps, 4 days a week. If you skip this, you’re just delaying the next injury.

Phase 3: The Run-Walk Protocol - Your First Steps Back
This is where most runners fail. They think ‘no pain, no gain’ applies here. It doesn’t. You need structure.
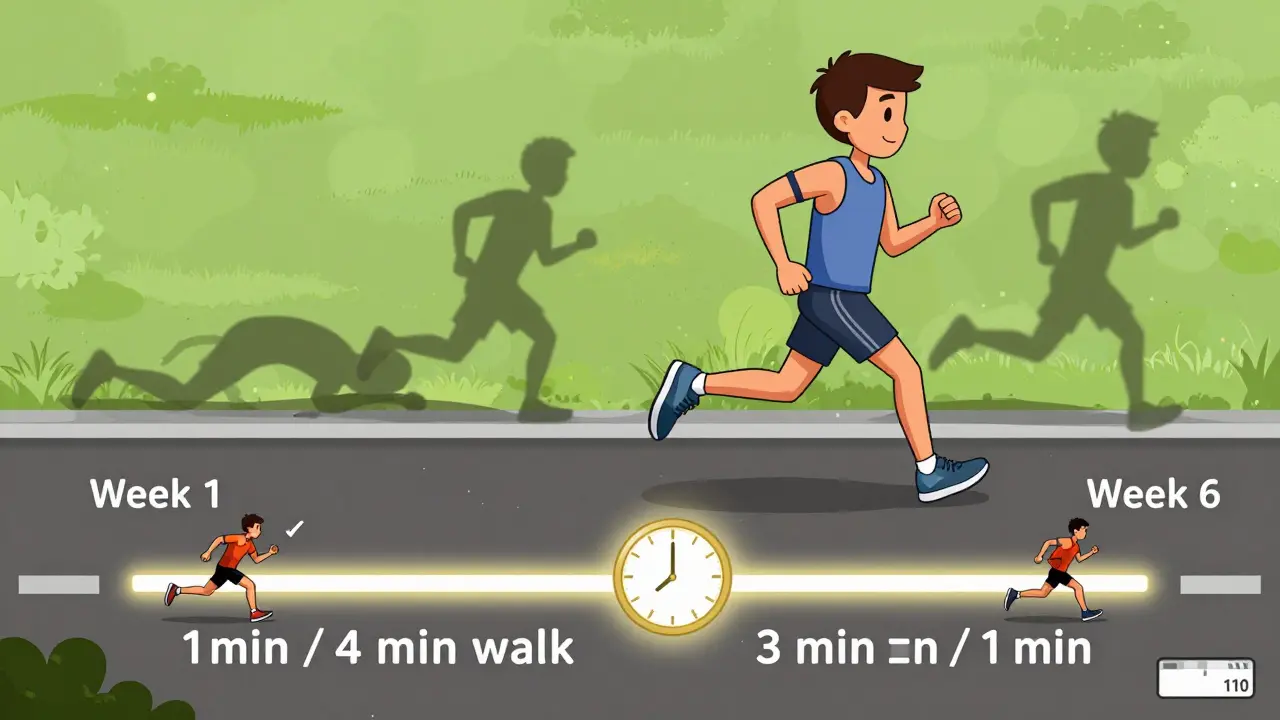
For low-risk stress fractures (posterior medial tibia), use the 6-week protocol:
- Week 1-2: 1 minute run, 4 minutes walk. Total: 20 minutes. Twice a week.
- Week 3: 1:3 ratio. 25 minutes total.
- Week 4: 1:2 ratio. 30 minutes total.
- Week 5: 1:1 ratio. 35 minutes total.
- Week 6: 3 minutes run, 1 minute walk. 40 minutes total.
For high-risk sites - like the front of the tibia or femoral neck - double the time. 8-12 weeks minimum.
And here’s the rule: if pain goes over 2/10 during or after, go back a step. Not tomorrow. Today. You don’t get credit for pushing through. You get a setback.
And no - the 10% weekly mileage increase doesn’t work for most people. A 2024 review found it’s inappropriate for 68% of runners with stress injuries. Your bone doesn’t care about percentages. It cares about load, recovery, and fuel.
Phase 4: Return to Full Running - Slow and Smart
Once you’ve completed the run-walk phase, don’t jump into your old routine. Start with 50% of your pre-injury mileage. Keep your pace easy. No intervals. No hills.
Use a 48-hour rule: if you run on Monday, don’t run again until Wednesday. Bone needs 48 hours to adapt. Studies show this cuts recurrence by 34%.
Track your pain daily. Use a 0-10 scale. If it’s above 1/10 the next morning, you did too much. Back off. Don’t be proud. Be smart.
After 4 weeks of consistent running at 50% mileage, increase by 10% every 10 days - not weekly. And always include at least one full rest day per week.
What Most Runners Get Wrong
Here’s what the data says about why people fail:
- Skipping hip work: 57% of those who re-injured never did glute exercises.
- Ignoring nutrition: 31% of female runners with repeat fractures had undiagnosed RED-S.
- Going too fast: 42% of recreational runners quit protocols because they rushed. One Reddit user said: ‘I jumped to 1:1 after 2 pain-free days. Got re-injured in 3 weeks.’
- Using heel lifts: They only reduce tibial strain by 12-15%. Gait retraining - like shortening your stride - reduces it by 38%.
And yes - you can use tech to help. WHOOP straps now track bone strain with 89% sensitivity. Apps like RunRx use AI to predict recovery time based on your training history, biomechanics, and even blood markers. But tech doesn’t replace discipline. It just makes it easier to stick to the plan.
When to See a Pro
If you’ve tried this and you’re still hurting - get help. A physical therapist who specializes in runners can:
- Check your gait with motion capture (used by 78% of NCAA programs)
- Assess your bone health with DXA scans
- Rule out hormonal imbalances
- Adjust your protocol based on real-time feedback
Insurance in the U.S. now covers up to 12 physical therapy sessions for stress injuries. That’s more than before. Use it.
Final Thoughts: Patience Isn’t Optional
Running isn’t just about miles. It’s about biology. Your bones need time. Your body needs fuel. Your mind needs patience.
Successful return-to-run plans have an 89% success rate - but only if you follow them. Miss a step. Skip the hip work. Push too soon. You’re not being tough. You’re being risky.
There’s no shortcut. But there is a path. And it’s clear: rest, rebuild, return - slowly, smartly, and with your eyes wide open.
Can I keep running if my shin splints hurt only a little?
No. Even mild pain is your body’s warning. Shin splints can turn into stress fractures if you keep loading the bone. Stop running and switch to low-impact cross-training until you’re completely pain-free for at least 7 days. Pain over 2/10 during activity means you’re stressing the tissue too much.
How long does it take to heal from a stress fracture?
Low-risk stress fractures (like the back of the shin) usually take 6-8 weeks to heal. High-risk sites - like the front of the tibia, femoral neck, or navicular - take 8-12 weeks. Bone doesn’t heal under load. You need full rest first, then a very gradual return. Rushing increases your chance of re-injury by up to 50%.
Should I use heel lifts or orthotics for shin splints?
Heel lifts and orthotics reduce tibial strain by only 12-15%. That’s not enough. Research shows gait retraining - like shortening your stride and increasing cadence - reduces strain by 38%. Focus on how you run, not what’s in your shoe. Strengthening your calves and hips is far more effective than any insert.
Is it safe to use a treadmill during recovery?
Yes - but only after you’re pain-free walking. Start with a 0% incline and slow speed. Use the run-walk protocol on the treadmill if you need to. Avoid high inclines or speed work. The treadmill can help you control load, but it’s not a magic fix. If you feel pain, stop. You’re still healing.
Why do some runners keep getting shin injuries even after resting?
Three main reasons: 1) They didn’t fix the root cause - weak hips or poor running form. 2) They returned too fast, skipping strength phases. 3) They’re under-fueled. Up to 31% of female runners with recurring injuries have RED-S - their body lacks energy to repair bone. Nutrition, sleep, and stress management are just as important as stretching and strengthening.
Can I do strength training while recovering?
Yes - and you should. Focus on calf raises (double-leg, then single-leg), hip abductions, glute bridges, and step-ups. Do these daily or every other day. Avoid anything that causes pain in your shins. Strength training rebuilds the support system around the bone. It’s not optional - it’s essential for preventing recurrence.
What’s the fastest way to get back to running?
There’s no fast way - only smart ways. The fastest recovery comes from strict adherence to the phases: rest first, then strength, then gradual running. Athletes who follow the full protocol return 22 days faster than those who self-manage. Using an anti-gravity treadmill (like AlterG) can cut recovery time by 27 days, but it’s not necessary. Discipline is.

PAUL MCQUEEN
February 8, 2026 AT 03:43Susan Kwan
February 9, 2026 AT 00:02Tricia O'Sullivan
February 10, 2026 AT 23:35MANI V
February 12, 2026 AT 14:45Andy Cortez
February 13, 2026 AT 07:54Tasha Lake
February 15, 2026 AT 04:35Frank Baumann
February 15, 2026 AT 06:19Jacob den Hollander
February 17, 2026 AT 03:58Brandon Osborne
February 18, 2026 AT 18:35Andrew Jackson
February 19, 2026 AT 05:15Chelsea Deflyss
February 19, 2026 AT 08:30Random Guy
February 19, 2026 AT 11:35Alex Ogle
February 20, 2026 AT 18:15