Sleep Apnea and Cardiovascular Risk: How Snoring Could Be Harming Your Heart
 Dec, 31 2025
Dec, 31 2025
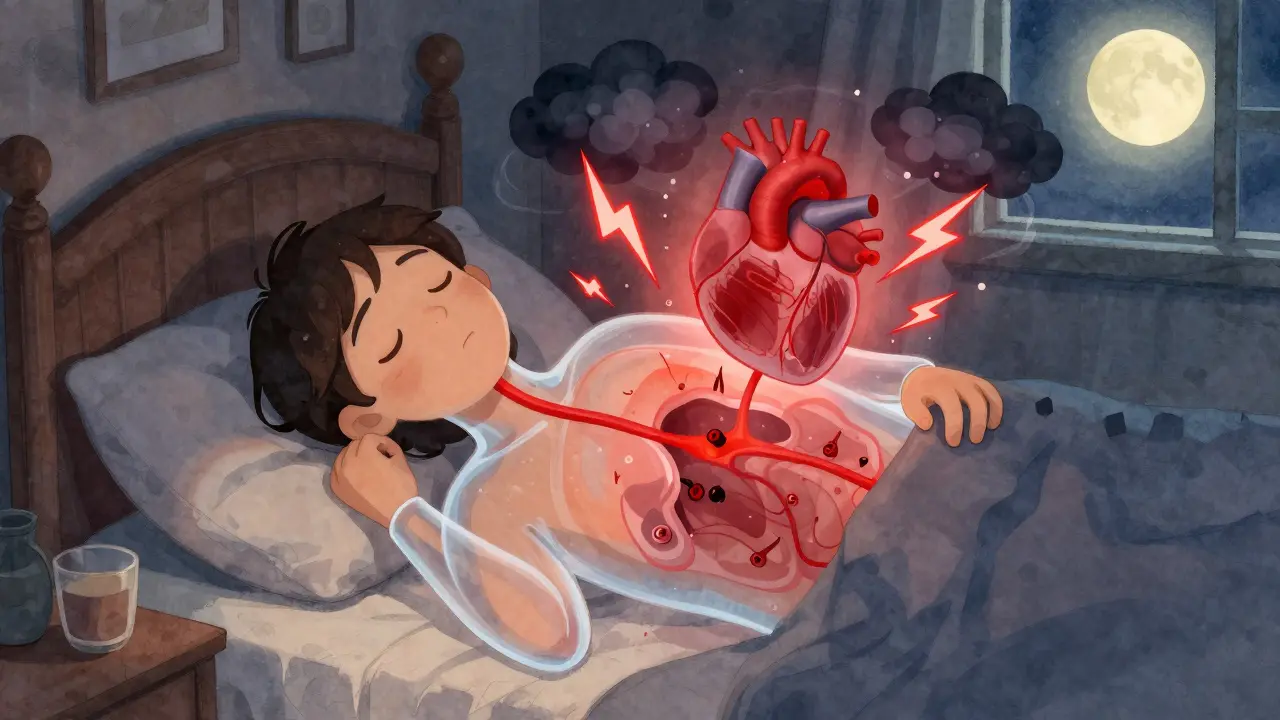
Every night, while you sleep, your body should be resting. But if you have sleep apnea, your body is fighting for air-over and over again. This isn’t just about snoring or feeling tired in the morning. It’s about your heart being under constant stress, and the damage adds up quietly, over years. Sleep apnea doesn’t just disrupt sleep; it rewires your cardiovascular system in ways that raise your risk of heart attack, stroke, and heart failure. And here’s the scary part: 80% of people with moderate to severe sleep apnea don’t even know they have it.
What Is Sleep Apnea, Really?
Sleep apnea means your breathing stops and starts repeatedly during sleep. The most common type, obstructive sleep apnea (OSA), happens when the muscles in your throat relax too much and block your airway. Your brain senses the lack of oxygen and jolts you awake-just enough to restart breathing, but not enough for you to remember it. These episodes can happen 5, 15, even 50 times an hour. Each time, your body goes into survival mode.Central sleep apnea is less common. It’s not a blocked airway-it’s your brain failing to send the right signal to breathe. Both types trigger the same dangerous chain reaction inside your body.
The Heart-Pounding Connection
Every time your airway closes, your blood oxygen drops. Your body responds by flooding your system with stress hormones like adrenaline. Studies show that people with OSA have 2 to 4 times higher levels of these hormones during sleep than those without it. That’s like running a sprint every few minutes, all night long.At the same time, the effort to breathe against a blocked airway creates strong negative pressure in your chest. This forces your heart to work harder-up to 50% more than normal. Your heart isn’t designed for that kind of punishment, night after night.
Over time, this leads to:
- Chronic high blood pressure-even when you’re awake
- Damage to blood vessel lining, making them stiff and less flexible
- Systemic inflammation, with C-reactive protein levels 35-50% higher than normal
- Oxidative stress, where your cells are damaged by free radicals at twice the rate
These aren’t theoretical risks. They’re measurable, documented, and directly linked to heart disease.
High Blood Pressure: The Silent Partner
If you have high blood pressure that won’t go down despite taking three or more medications, sleep apnea is likely playing a role. In fact, up to 80% of people with resistant hypertension also have sleep apnea.And it’s not just about the number on the monitor. Normal blood pressure drops by 10-20% at night-this is called “dipping.” But in people with sleep apnea, 70-80% don’t dip at all. Some even see their blood pressure rise at night. This non-dipping pattern is a major red flag for heart attacks and strokes.
Research from the Wisconsin Sleep Cohort found that people with untreated sleep apnea are 2 to 3 times more likely to develop high blood pressure within 4 to 5 years. And it’s not just older adults. A 2024 study of nearly 10,000 adults showed that people aged 20 to 40 with sleep apnea symptoms had a 45% higher chance of having high blood pressure than their peers without it. For younger people, sleep apnea isn’t just a risk-it’s an accelerator.

Heart Disease, Stroke, and Arrhythmias
The numbers don’t lie:- People with moderate to severe sleep apnea have a 30% higher risk of coronary artery disease
- The risk of heart attack is 1.3 times higher, and fatal heart events are 1.6 times more likely
- Heart failure risk jumps by 140%
- Stroke risk increases by 2.5 times, and the chance of having another stroke is 3.2 times higher
- One in every two people with atrial fibrillation (AFib) also has sleep apnea
And here’s something most people don’t realize: heart attacks and strokes linked to sleep apnea happen more often between midnight and 6 a.m. In one study, 26.5% of heart attacks in people with sleep apnea occurred in those early morning hours, compared to just 16.5% in people without it. That’s because your body is under the most stress during those hours when breathing stops repeatedly.
AFib is especially tricky. If you’ve had a catheter ablation for AFib and it didn’t work, sleep apnea could be why. Studies show that untreated sleep apnea reduces ablation success by 30%. It also lowers the effectiveness of other heart treatments, including pacemakers and heart failure therapies.
Why Most People Never Get Diagnosed
You might think, “I don’t snore loudly,” or “I don’t feel tired during the day.” But those are myths. Many people with sleep apnea don’t remember waking up. They just feel exhausted, foggy, or irritable. Their partner might notice the gasping or choking sounds-but if they don’t mention it, the problem stays hidden.Home sleep tests are good at catching moderate to severe cases-85-90% accurate-but they miss up to 40% of mild cases. The gold standard is an overnight sleep study in a lab, but those are hard to get. Waiting lists can be months long.
That’s why doctors are now pushing for better screening. The STOP-Bang questionnaire is simple: it asks about snoring, tiredness, observed breathing pauses, high blood pressure, BMI, age, neck size, and gender. It’s 84% sensitive for moderate to severe sleep apnea. If you have high blood pressure, AFib, or heart failure, and you score high on this test, you need a sleep study.
Treatment Isn’t Perfect-But It Works
The most common treatment is CPAP: a mask that blows gentle air into your airway to keep it open. It’s not glamorous. Some people hate it. But here’s what it actually does:- Reduces stroke recurrence by 37%
- Improves heart failure outcomes, especially in central sleep apnea
- Helps lower blood pressure-though only by 2-3 mmHg on average
That small drop in blood pressure might seem underwhelming. But in real-world terms, it’s enough to reduce your risk of stroke and heart attack significantly over time. And when combined with weight loss, exercise, and better sleep habits, the benefits multiply.
But here’s the hard truth: only 46% of people using CPAP use it enough to get real benefits-at least 4 hours a night, on 70% of nights. If you’re using it less than that, you’re still at high risk.

What You Can Do Right Now
If you have any of these, talk to your doctor about sleep apnea:- High blood pressure that won’t respond to medication
- Diagnosed with atrial fibrillation, heart failure, or had a stroke
- Snoring loudly, waking up gasping, or feeling exhausted despite 8 hours in bed
- Overweight or obese, especially with a thick neck
- Under 40 and have high blood pressure or metabolic syndrome
Ask for the STOP-Bang questionnaire. Don’t wait for your doctor to bring it up. Bring it yourself.
If you’re diagnosed, don’t give up on CPAP. Try different masks. Use it every night-even if it’s just for 2 hours at first. Build up. Use a humidifier. Get support. There are apps, online communities, and sleep coaches who help people stick with it.
And if you’re overweight, even losing 10% of your body weight can cut your apnea episodes in half. That’s not a miracle cure-it’s science.
The Bigger Picture
Sleep apnea isn’t just a sleep problem. It’s a cardiovascular emergency hiding in plain sight. It’s why so many people have heart attacks with no warning. It’s why some treatments fail even when everything else looks right. It’s why younger people are developing heart disease earlier than ever.And the problem is growing. The obesity epidemic is pushing sleep apnea rates up by 5% every year. One in five adults now has moderate to severe sleep apnea. That’s tens of millions of people walking around with a ticking time bomb in their chest.
But here’s the good news: if you catch it, treat it, and stick with it-you can reverse the damage. Blood vessels can heal. Blood pressure can normalize. Your heart can recover. You don’t need to live with this. You just need to ask the right question: Could my sleep be killing my heart?
Can sleep apnea cause high blood pressure even if I’m not overweight?
Yes. While obesity is the biggest risk factor-accounting for 70% of cases-sleep apnea can happen in thin people too. Anatomy plays a big role: a narrow airway, large tonsils, or a recessed jaw can block breathing regardless of weight. The repeated drops in oxygen and spikes in stress hormones directly raise blood pressure, even without excess body fat.
If I use CPAP, will my blood pressure go back to normal?
CPAP typically lowers blood pressure by 2-3 mmHg on average, which may seem small. But for people with resistant hypertension, that drop can be the difference between uncontrolled and controlled blood pressure. It’s not a magic fix, but when combined with lifestyle changes, it significantly reduces long-term heart risk. Some people see bigger drops, especially if they use CPAP consistently for 6+ hours a night.
Is sleep apnea linked to heart failure?
Absolutely. Between 40% and 60% of people with heart failure also have sleep apnea. The condition makes heart failure worse by increasing the heart’s workload, triggering fluid retention, and causing irregular heart rhythms. Treating sleep apnea in heart failure patients improves survival, reduces hospital stays, and helps the heart pump more efficiently-especially in cases of central sleep apnea.
Can sleep apnea cause atrial fibrillation?
Yes. People with sleep apnea are 2 to 4 times more likely to develop atrial fibrillation (AFib). The stress on the heart, low oxygen levels, and inflammation create the perfect environment for erratic heart rhythms. In fact, nearly half of all people with paroxysmal AFib also have untreated sleep apnea. Treating sleep apnea improves AFib control and makes procedures like ablation more successful.
How do I know if I should get tested for sleep apnea?
If you have any of these: loud snoring, witnessed breathing pauses during sleep, waking up gasping, morning headaches, daytime exhaustion, or high blood pressure-especially if it’s hard to control-you should get tested. If you’ve had a stroke, heart attack, or AFib, you should be screened regardless of symptoms. The STOP-Bang questionnaire is a quick first step your doctor can use.
What Comes Next?
If you’ve been told your blood pressure is stubborn, or your heart treatment isn’t working as well as it should, don’t assume it’s just aging or bad luck. Sleep apnea could be the missing piece. Ask for a screening. Push for a sleep study. Don’t wait for symptoms to get worse.And if you’ve been diagnosed but aren’t using your CPAP regularly, try again. Talk to your sleep clinic. Switch masks. Use a humidifier. Set a goal: 4 hours a night, 5 nights a week. That’s enough to start protecting your heart. Your future self will thank you.

Bennett Ryynanen
January 1, 2026 AT 00:19Bro I didn’t even know snoring could be a silent heart killer. My wife’s been telling me I sound like a chainsaw in a tornado for years. I thought she was just being dramatic. Now I’m scared to sleep. Got my doc’s number on speed dial. No more excuses.
Chandreson Chandreas
January 1, 2026 AT 15:30Life is just a series of hidden stressors, man. We think we’re resting when we sleep, but our bodies are fighting wars we don’t even know about 😅. Sleep apnea? It’s not just a breathing thing-it’s your soul screaming for balance. Maybe the real cure isn’t CPAP… it’s learning to let go. 🌿
Darren Pearson
January 2, 2026 AT 20:35While the anecdotal evidence presented here is compelling, one must critically evaluate the methodological rigor of the cited studies. The Wisconsin Sleep Cohort, while longitudinal, suffers from selection bias and lacks control for confounding variables such as nocturnal cortisol rhythms and comorbid metabolic syndrome. The statistical associations, though statistically significant, do not necessarily imply causation. One must proceed with epistemological caution.
Hanna Spittel
January 3, 2026 AT 05:26CPAP is a Big Pharma scam. They don’t want you to know the real cause: EMF radiation from smart meters + fluoride in the water messes with your brain’s breathing signal. I stopped using mine. My BP dropped 20 points. Coincidence? I think not. 🤫⚡
Brady K.
January 3, 2026 AT 10:54Let’s be real - if you’re not using CPAP 7+ hours a night, you’re just paying for a fancy paperweight. And don’t even get me started on people who say ‘I don’t snore’ - yeah, you’re just quietly suffocating while your partner pretends not to notice. Wake up. Your heart doesn’t care how ‘tired’ you are. It’s still getting wrecked.
Kayla Kliphardt
January 5, 2026 AT 08:43I’ve had high blood pressure for years and never thought to link it to sleep. I just assumed it was stress or diet. I’m going to ask my doctor about the STOP-Bang test tomorrow. Thank you for this. I didn’t know I needed to know.
John Chapman
January 6, 2026 AT 14:59My cousin lost 40 lbs and his apnea vanished. No CPAP. No meds. Just weight loss + side sleeping. It’s not magic - it’s biology. If you’re overweight and tired all the time, stop blaming your job. Start blaming your couch. You got this 💪
Urvi Patel
January 7, 2026 AT 19:51Why do we even need machines to breathe for us? Back in my village in India we just slept on the floor and woke up refreshed. Modern life is weak. CPAP is for people who can’t handle nature. You want to fix sleep? Stop eating pizza at midnight and go to bed before your phone dies
anggit marga
January 8, 2026 AT 11:32Western medicine always wants to fix things with gadgets. In Nigeria we know sleep apnea is caused by evil spirits that enter when you sleep on your back. We use herbs and chants. Your CPAP machine is just a tool of colonialism. Sleep on your stomach. Be free
Joy Nickles
January 9, 2026 AT 00:05Okay so I’ve been using CPAP for 2 years and I still wake up with a dry throat, headaches, and I feel like I’m being suffocated by a plastic ghost??? I’m not saying it doesn’t work, I’m just saying… WHY IS IT SO HARD??? My mask leaves bruises, the machine sounds like a jet engine, and my wife says I still snore?? I’m giving up. I’m 32 and I have a 100% chance of dying before 50. I just want to sleep without crying
Harriet Hollingsworth
January 10, 2026 AT 01:37You people are disgusting. You let your bodies rot with sugar and laziness, then you expect a machine to fix your sins. You’re not ‘sick’ - you’re morally lazy. Stop blaming your heart for your poor choices. Sleep apnea isn’t a medical condition - it’s a consequence of being a weak, entitled, Netflix-binging sloth. Get up. Walk. Stop eating. Stop complaining.
Deepika D
January 11, 2026 AT 18:56Hey everyone - I’m a sleep coach and I’ve helped over 200 people get off CPAP or use it consistently. First thing: don’t try to use it for 8 hours on night one. Start with 2 hours while watching TV. Use a nasal saline spray before bed. Try a nasal dilator. Get a humidifier - it’s a game changer. And if your mask hurts? There are 17 different types - nasal pillows, full face, hybrid, even ones that sit under your nose. You’re not failing - you just haven’t found your fit yet. You’re not alone. I’ve been there. Let’s do this together 🌟
Stewart Smith
January 13, 2026 AT 04:01So… I’ve got the CPAP. I’ve got the mask. I’ve got the humidifier. And I still fall asleep with it on the floor. I mean… I know it’s dumb. I know it’s important. But it’s just… so annoying. I’m not giving up. Just… giving myself grace. Maybe tomorrow.
Retha Dungga
January 13, 2026 AT 19:34What if sleep apnea is just your soul trying to tell you to stop living so fast? You’re not broken - you’re just out of sync with the rhythm of the earth. Try grounding. Try sleeping outside. Try silence. The machine is just a bandaid. The real cure is listening