Stroke Types: Ischemic vs. Hemorrhagic and How to Prevent Them
 Feb, 21 2026
Feb, 21 2026
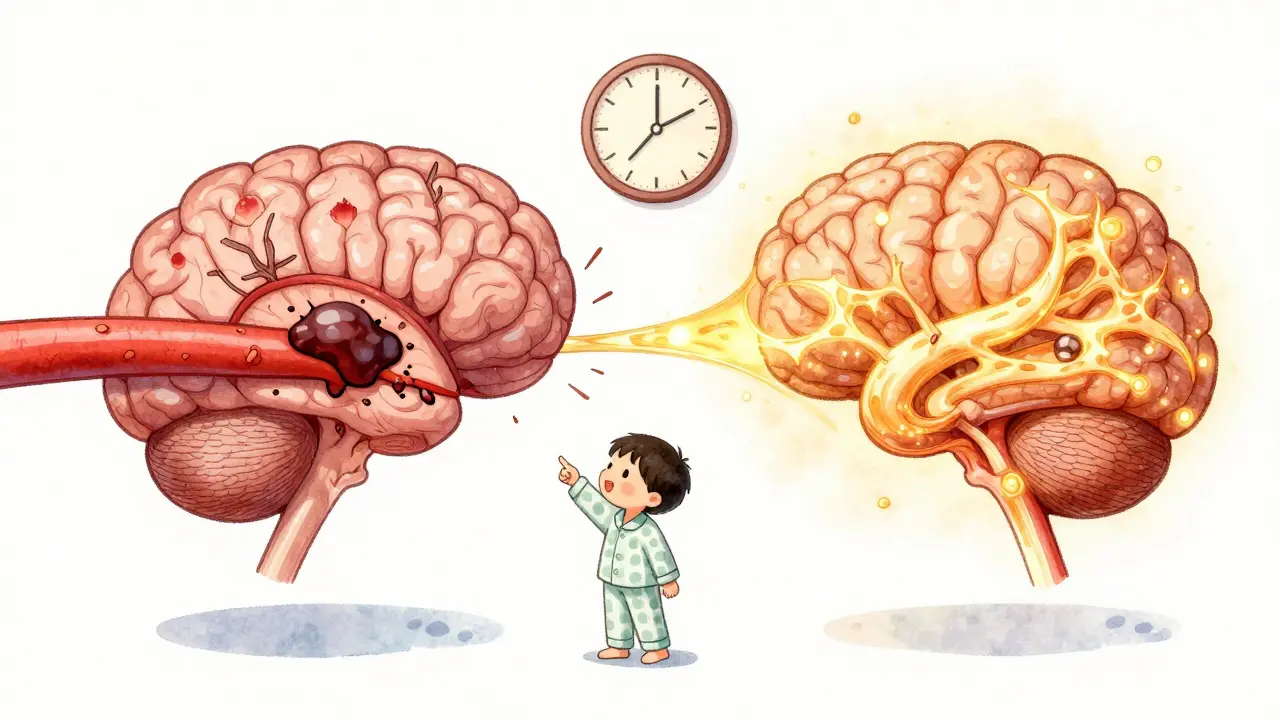
When someone has a stroke, every second counts. But not all strokes are the same. Two main types - ischemic and hemorrhagic - behave differently, need different treatments, and come from different causes. Knowing the difference isn’t just medical jargon; it can save a life. In the UK, stroke is the fourth leading cause of death, and nearly 100,000 people have one each year. Most of them - about 87% - have an ischemic stroke. The rest, around 13-15%, suffer a hemorrhagic stroke. Both are emergencies, but how you respond depends entirely on which one it is.
What Is an Ischemic Stroke?
An ischemic stroke happens when a blood clot blocks blood flow to part of the brain. Without oxygen, brain cells start dying within minutes. This is the most common type of stroke, making up nearly nine out of every ten cases.
There are three main kinds of ischemic strokes:
- Thrombotic strokes - the clot forms right inside an artery in the brain. About half of all ischemic strokes are like this, often linked to fatty buildup (atherosclerosis) in large arteries.
- Embolic strokes - the clot forms elsewhere, usually in the heart, and travels through the bloodstream until it gets stuck in a smaller brain artery. This is common in people with atrial fibrillation (AFib), a type of irregular heartbeat.
- Cryptogenic strokes - no clear cause is found after testing. These make up about 30% of ischemic strokes and are especially tricky because you can’t target the exact cause without more data.
Symptoms usually come on slowly. Someone might notice their arm going numb, then their speech gets slurred, and over 15 to 30 minutes, it gets worse. Many people think it’s just tiredness or a migraine. That’s dangerous. The FAST test is simple: Face drooping? Arm weakness? Speech difficulty? Time to call 999. If you see any of these, act fast.
What Is a Hemorrhagic Stroke?
A hemorrhagic stroke is when a blood vessel in the brain bursts and bleeds into or around the brain tissue. This type is less common - only about 1 in 7 strokes - but it’s often more deadly. The bleeding increases pressure in the skull, crushing brain tissue and cutting off oxygen.
There are two main forms:
- Intracerebral hemorrhage - bleeding directly into the brain. This is the most common type of hemorrhagic stroke, and it’s strongly tied to high blood pressure. In fact, 78% to 88% of these cases happen because of uncontrolled hypertension.
- Subarachnoid hemorrhage - bleeding on the surface of the brain, usually from a ruptured aneurysm. This is the kind that causes the infamous "thunderclap headache" - a sudden, explosive pain described by survivors as "the worst headache of my life."
The symptoms hit like a sledgehammer. Unlike ischemic strokes, hemorrhagic strokes often come on instantly. People report losing consciousness, vomiting, having seizures, or seeing double. One study found that 92% of hemorrhagic stroke patients had a severe headache - compared to just 19% of ischemic stroke patients. Pupils may become unequal or dilated. Agitation and confusion are common. These signs are harder to ignore - but they’re also harder to recognize unless you know what to look for.
How Are They Treated Differently?
Here’s where it gets critical: giving the wrong treatment can kill someone.
If it’s an ischemic stroke, doctors try to dissolve or remove the clot. The gold standard is a drug called alteplase (tPA), given through an IV. But it only works if given within 4.5 hours of symptom onset. A newer drug, tenecteplase, is now approved in the UK and US, and it’s slightly more effective with fewer side effects. For larger clots in major brain arteries, a mechanical thrombectomy - a tiny device pulled through the groin to grab and remove the clot - can be done up to 24 hours after the stroke starts. Studies show this can restore blood flow in over 80% of cases when done quickly.
If it’s a hemorrhagic stroke, you can’t give clot-busting drugs. That would make the bleeding worse. Instead, doctors focus on stopping the bleed, lowering pressure in the skull, and fixing the source. If it’s an aneurysm, they might do a coiling procedure - threading a tiny coil through the artery to seal the weak spot - or a surgical clip, where a metal clip is placed over the aneurysm to stop the leak. For bleeding inside the brain, a new technique called MISTIE uses a small tube to drain the blood and flush it with clot-dissolving medicine. This reduced death rates by 10% in recent trials.
CT scans are the first test used in emergency rooms to tell the difference. But new blood tests are on the horizon. A biomarker called GFAP, found in blood samples, can now distinguish hemorrhagic from ischemic stroke with 92% accuracy within 15 minutes. This could change how ambulances and rural clinics respond before even reaching the hospital.

What Causes Each Type?
Understanding the root cause is the key to prevention.
Ischemic stroke is closely linked to heart and artery problems:
- Atrial fibrillation (AFib) - irregular heartbeat - increases stroke risk by 5 times. People with AFib are often put on blood thinners like apixaban or warfarin, which cut stroke risk by 60-70%.
- High cholesterol and smoking lead to plaque buildup in arteries.
- Diabetes and obesity raise the risk of clots forming.
Hemorrhagic stroke is mostly about pressure:
- High blood pressure is the #1 cause. Keeping systolic pressure below 120 mmHg (not 140) cuts hemorrhagic stroke risk by 38%, according to the SPRINT trial.
- Smoking weakens blood vessel walls.
- Excessive alcohol use raises blood pressure and can trigger bleeding.
- Use of blood thinners (like warfarin) can increase bleeding risk if not monitored carefully.
How to Prevent a Stroke - Type-Specific Strategies
Prevention isn’t one-size-fits-all. You need to target the type of stroke you’re most at risk for.
For ischemic stroke prevention:
- If you have AFib, take your prescribed blood thinner. Don’t skip doses. Studies show people who miss even one pill a week have double the stroke risk.
- Take low-dose aspirin (81mg) daily if you’ve had a prior stroke or TIA - it cuts recurrence by 25%.
- Manage cholesterol with statins. Lowering LDL to under 70 mg/dL reduces plaque buildup.
- Exercise 150 minutes a week. Walking, cycling, swimming - even light activity reduces stroke risk by 27%.
For hemorrhagic stroke prevention:
- Monitor your blood pressure daily. Use a home monitor. If it’s above 130/80, talk to your doctor. Don’t wait for symptoms.
- Reduce salt intake. Aim for under 1,500mg of sodium per day. The Mediterranean diet - rich in olive oil, nuts, fish, and vegetables - has been shown to cut stroke risk by 30%.
- Quit smoking. Within one year of quitting, stroke risk drops by half. No delay.
- Limit alcohol. More than one drink a day for women, two for men, raises bleeding risk.
Both types benefit from:
- Controlling diabetes
- Maintaining a healthy weight
- Getting regular check-ups

What Survivors Say - Real Stories
On patient forums, ischemic stroke survivors often say: "I thought I was just tired. My arm went numb, and my words got tangled. I waited 20 minutes before calling. That’s when I lost the chance to get tPA."
Hemorrhagic stroke survivors say: "I felt like my head was splitting open. I blacked out. My wife said I was screaming. She called 999 right away. That’s why I’m here."
One man in Bristol, 58, had no history of heart disease. His blood pressure was 145/90 - he thought it was "fine." He had a hemorrhagic stroke. His recovery took 18 months. "I didn’t know high blood pressure could kill you like that," he told his doctor. "Now I check it every morning. I’m alive because I listened."
Another woman, 67, had AFib. She stopped her apixaban because she didn’t like the monthly blood tests. Six months later, she had an ischemic stroke. She survived, but now has trouble walking. "I thought I was fine. I didn’t realize the risk was still there."
What’s Changing in Stroke Care
Technology is making stroke care faster and smarter. AI tools like Viz.ai now scan brain scans in seconds, alerting hospitals before the patient even arrives. This cuts "door-to-needle" time for tPA by over 50 minutes. In 2023, the UK rolled out telestroke networks to rural areas - meaning a neurologist in London can guide a local ER doctor through a stroke diagnosis in real time.
Research is also shifting. The WAKE-UP trial showed that MRI scans can identify brain tissue still at risk - even 9 hours after symptoms start. This means more people might qualify for clot-busting drugs than we thought.
And blood tests for GFAP? They’re being tested in ambulances. Imagine: paramedics draw a vial of blood, get a result in 10 minutes, and know whether to head straight to a neurosurgery center. That’s not science fiction - it’s happening now.
Final Takeaway
Ischemic and hemorrhagic strokes are not the same. One is a clogged pipe. The other is a burst pipe. You fix them differently. But both need you to act fast - and prevent them before they happen.
Know your numbers: blood pressure, cholesterol, heart rhythm. Take your meds. Quit smoking. Move daily. If someone shows signs of stroke - even if they seem "not that bad" - call 999. Don’t wait. Don’t guess. Don’t hope it goes away. Your brain is losing 1.9 million neurons every minute. That’s not a statistic - it’s real time ticking away.
What’s the difference between ischemic and hemorrhagic stroke?
An ischemic stroke happens when a blood clot blocks blood flow to the brain, while a hemorrhagic stroke occurs when a blood vessel bursts and causes bleeding inside or around the brain. Ischemic strokes make up 87% of cases; hemorrhagic strokes make up 13-15%. They require completely different treatments - one needs clot removal, the other needs bleeding control.
Can you have a stroke and not know it?
Yes - especially with small ischemic strokes called "silent strokes." These don’t cause obvious symptoms like weakness or slurred speech, but they damage brain tissue and increase the risk of a major stroke later. They’re often found by accident on an MRI or CT scan done for another reason. That’s why checking blood pressure and heart rhythm regularly matters, even if you feel fine.
Is aspirin good for stroke prevention?
Aspirin (81mg daily) helps prevent a second ischemic stroke or TIA by reducing clot formation. But it’s not for everyone. If you’ve never had a stroke, or if you have uncontrolled high blood pressure or a history of bleeding, aspirin can do more harm than good. Always talk to your doctor before starting daily aspirin.
Can hemorrhagic stroke be prevented?
Yes - by controlling high blood pressure. Keeping systolic pressure below 120 mmHg cuts hemorrhagic stroke risk by 38%. Quitting smoking, limiting alcohol, and avoiding blood thinners unless necessary also help. Regular check-ups and home blood pressure monitoring are key.
What should I do if I think someone is having a stroke?
Use the FAST test: Face drooping? Arm weakness? Speech difficulty? Time to call 999. Don’t wait. Don’t drive them yourself. Call emergency services immediately. Every minute counts. If the person is unconscious, place them on their side and keep them warm until help arrives.
