Taking Medications with Food: How Timing Affects Absorption and Effectiveness
 Nov, 17 2025
Nov, 17 2025
Did you know that taking your pill with breakfast could make it work worse-or even cause dangerous side effects? It’s not just about swallowing a pill. Food-drug interactions can change how your body absorbs medication, turning a helpful treatment into a wasted dose-or worse, a health risk.
Why Food Changes How Medicines Work
When you eat, your body shifts into digestion mode. Stomach acid levels drop. Gastric emptying slows down. Bile flows to break down fats. All of this affects how drugs move through your system. For some medications, food helps. For others, it blocks absorption. A high-fat meal can delay gastric emptying by up to two hours, meaning a pill might sit in your stomach longer instead of moving to the small intestine where most drugs are absorbed. That’s why some drugs peak in your blood 45 minutes after taking them on an empty stomach-but take over 90 minutes if you ate a fatty meal. The science behind this is well-documented. The FDA requires drug makers to test how food affects absorption before approval. If a drug’s bioavailability changes by more than 20% when taken with food, the label must say so. About 35% of new drugs approved between 2015 and 2022 have food-effect warnings on their labels.When Food Helps: Drugs That Need a Meal
Not all medications are better on an empty stomach. Some actually need food to work at all. Griseofulvin, an antifungal used for nail infections, absorbs 200-300% better when taken with a high-fat meal. Why? Fat triggers bile release, which helps dissolve the drug so your body can absorb it. Nitrofurantoin, a common antibiotic for urinary tract infections, sees a 40% increase in absorption when taken with food. This isn’t just helpful-it’s necessary to reach effective blood levels. Cefpodoxime, another antibiotic, absorbs 50-60% better with food. Without it, you might not get enough of the drug into your system to kill the infection. Even GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) are affected. Taking them within 30 minutes of eating reduces absorption by 44%, which can lower their effectiveness for weight loss or blood sugar control. That’s why experts recommend waiting at least 30 minutes after taking it before eating.When Food Hurts: Drugs That Need an Empty Stomach
Some medications are sabotaged by food-even healthy food. Levothyroxine, used for hypothyroidism, is one of the most critical. Food can reduce its absorption by 30-55%. That means you might still feel tired, gain weight, or have high cholesterol-even if you’re taking the right dose. The rule? Take it on an empty stomach, at least 30-60 minutes before breakfast, with plain water only. Coffee, juice, and even mineral water can interfere too. Tetracycline antibiotics like doxycycline bind to calcium, magnesium, and iron. That means dairy products, antacids, and iron supplements can block up to 75% of absorption. One Reddit user reported a recurring UTI that didn’t clear until they stopped taking doxycycline with yogurt. Two hours before or after dairy was the fix. Itraconazole, an antifungal, needs stomach acid to dissolve. High-fat meals raise stomach pH, making it harder for the drug to dissolve. This can cut absorption by 40%. The fix? Take it with an acidic drink like cola, and avoid heavy meals. Sulfonylureas like glipizide stimulate insulin release. If taken on an empty stomach, they can cause dangerous low blood sugar (below 70 mg/dL). In fact, 23% of patients who take these diabetes pills without food experience symptoms like shaking, sweating, or confusion. The solution? Take them 30 minutes before eating.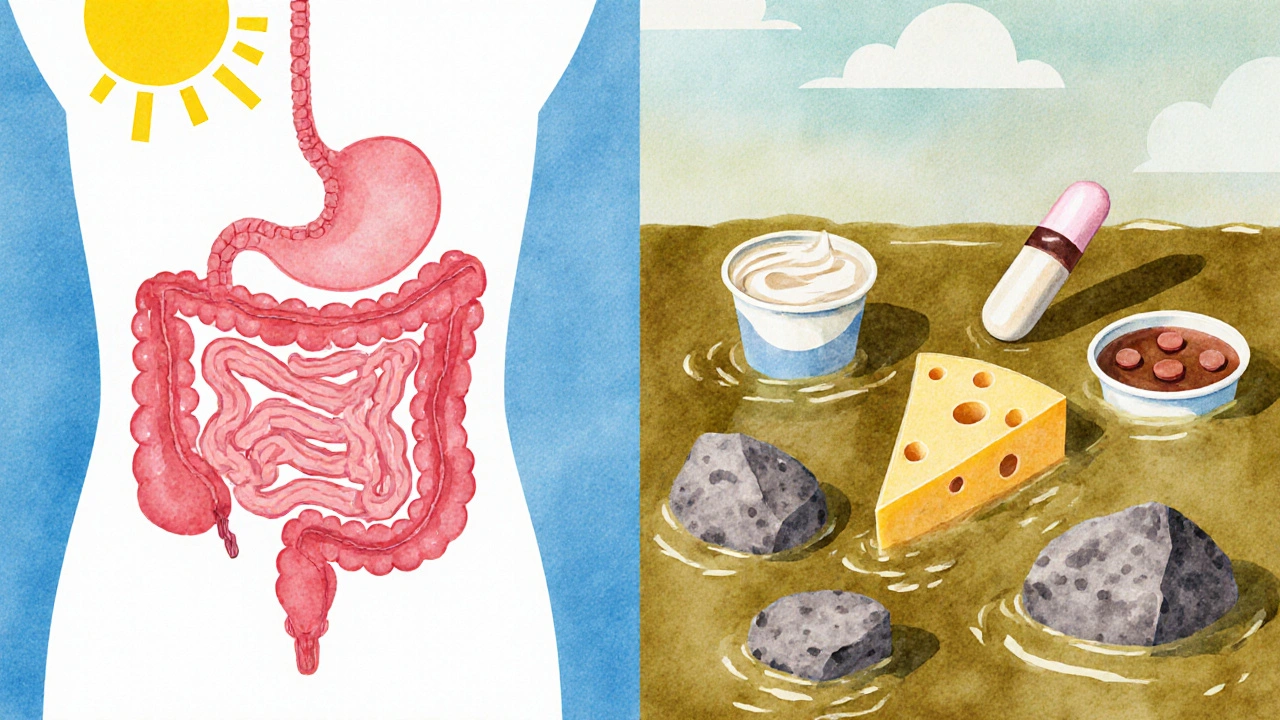
What Does “With Food” Really Mean?
Many people think “take with food” means a full meal. That’s not always true. For some drugs, like certain antiretrovirals used for HIV, a small snack of 200-300 calories is enough to prevent stomach upset without affecting absorption. A banana, a handful of crackers, or a yogurt cup can be sufficient. The Australian Prescriber defines “with food” as taking the medication within 30 minutes of starting your meal. That’s the window where food is still actively influencing digestion. Taking it an hour after finishing your meal? That’s too late. A 2023 Express Scripts report found that 45% of patients misunderstand this instruction. One woman took her HIV meds with a full dinner every night-but she ate dinner at 9 p.m. She felt nauseous every time. The fix? Switching to a light snack at 7 p.m., right before her pill. Her side effects vanished.Why Timing Matters More Than You Think
It’s not just about whether you eat. It’s about consistency. If you take your levothyroxine one day before breakfast, another day after, and skip it on weekends, your thyroid hormone levels will swing wildly. That’s why doctors stress routine: same time, same conditions, every day. For chronic medications, especially those for high blood pressure, cholesterol, or depression, the goal isn’t always maximum absorption-it’s stable, predictable levels. A slight delay in absorption doesn’t matter if the total amount absorbed stays the same. But for drugs like levothyroxine, antibiotics, or antifungals, even small changes in absorption can mean treatment failure. That’s why the Mayo Clinic says timing matters for about 25% of commonly prescribed drugs.Who’s Most at Risk?
Older adults are the most vulnerable. Nearly half of adults over 65 take five or more medications. Each one adds another chance for a food interaction. A 2022 study in the Journal of the American Geriatrics Society found that people on five or more drugs have a 65% higher risk of food-drug interactions. That’s not just a number-it’s a real risk of hospitalization, falls from low blood sugar, or infections that don’t clear. People on special diets-vegan, gluten-free, low-fat-are also at risk. Standard food-effect studies used high-fat meals. But if you’re eating a plant-based diet, the interaction might be different. The FDA now recommends testing with diverse meal types, including plant-based options, to reflect modern eating habits.
How to Get It Right
Here’s how to avoid mistakes:- Ask your pharmacist: “Should I take this with food, before food, or after?” Don’t assume.
- Set phone alarms. If you take levothyroxine before breakfast, set a reminder for 60 minutes before you eat.
- Use a pill organizer with time labels. Some apps like Medisafe and MyTherapy have built-in food-timing reminders.
- Keep a simple log: Note what you ate and when you took your meds. If symptoms change, you’ll spot patterns.
- Don’t mix calcium-rich foods with tetracycline, iron supplements, or thyroid meds. Wait two hours.
- If you forget and take a pill with food, don’t double up. Just take the next dose at the right time.
The Bigger Picture: Cost, Safety, and Innovation
Food-drug interactions aren’t just a personal problem-they’re a system-wide issue. In the U.S., medication-related problems cost $528 billion a year. Food interactions alone account for about 8% of that-roughly $42 billion. That includes hospital visits, ER trips, and failed treatments. New tools are emerging. Ingestible sensors that track stomach pH and emptying are being tested. One 2023 trial showed a 38% improvement in absorption consistency for pH-sensitive drugs when patients got real-time feedback on timing. Also, research in Nature Medicine (March 2024) shows that combining food timing with circadian rhythms-taking certain meds at the same time each day, based on your body’s natural clock-can improve effectiveness by up to 30%.Bottom Line: Don’t Guess. Ask.
Food isn’t just fuel. It’s part of your medication regimen. Taking a pill the wrong way can mean it doesn’t work-or makes you sick. If you’re on more than one medication, especially for chronic conditions, review your list with your pharmacist every six months. Ask specifically about food interactions. Write it down. Set reminders. Stick to the schedule. Your body doesn’t care if you’re busy, tired, or in a rush. It reacts to what you give it-and when. Get the timing right, and you’re not just taking medicine. You’re making it work.Can I take my medication with coffee or juice?
It depends on the medication. Coffee and citrus juices can interfere with some drugs. For example, grapefruit juice can block the breakdown of statins, blood pressure meds, and some anti-anxiety drugs, leading to dangerous buildup in your blood. Coffee can reduce absorption of levothyroxine. Water is the safest choice unless your doctor or label says otherwise.
What if I forget and take my pill with food?
Don’t double the dose. If you’re supposed to take it on an empty stomach but ate first, wait until your next scheduled dose and take it correctly then. For drugs like levothyroxine or antibiotics, one mistake won’t ruin your treatment-but doing it often will. Talk to your pharmacist if it happens frequently.
Does it matter if I take my pill with a snack versus a full meal?
For some drugs, yes. For others, no. Antibiotics like nitrofurantoin need food to absorb properly, but a light snack (200-300 calories) is enough. For drugs like levothyroxine, even a small snack can reduce absorption. Always follow the label or your pharmacist’s advice-don’t guess.
Why do some pills say “take with food” and others say “take on an empty stomach”?
It’s about how the drug behaves in your body. Some drugs need fat or acid to dissolve. Others get blocked by calcium, iron, or stomach contents. Manufacturers test these interactions during development. The label tells you what works best based on science-not opinion.
Can I take my vitamins with my medications?
Be careful. Iron, calcium, and magnesium supplements can block antibiotics like tetracycline and thyroid meds. Multivitamins often contain these minerals. Take them at least two hours apart from your medication. Always check with your pharmacist before combining supplements and prescriptions.

steffi walsh
November 18, 2025 AT 11:12Y’all need to stop treating meds like candy. I used to take my levothyroxine with my morning coffee because ‘it’s just water,’ and then spent six months feeling like a zombie. Switched to water only, 60 mins before breakfast? Life changed. Don’t be that person.
Also-yes, grapefruit juice is a silent killer for statins. I learned this the hard way. 😅
Kristina Williams
November 19, 2025 AT 01:06THEY DON’T WANT YOU TO KNOW THIS. Big Pharma doesn’t tell you that food ruins your meds because they make more money when you keep getting sick. I read a whistleblower report once-this stuff is buried in footnotes. They’d rather you take more pills than fix the timing. Wake up.
Also, did you know the FDA gets funding from drug companies? Coincidence? I think not.
Holly Powell
November 19, 2025 AT 13:20Let’s be real: the entire ‘take with food’ paradigm is a lazy clinical shortcut. The pharmacokinetic models are built on 1980s high-fat Western diets. What about a keto patient? A vegan? A fasting Muslim? The data is obsolete. This isn’t science-it’s institutional inertia wrapped in a label.
And don’t get me started on ‘light snack.’ Who defines that? A banana? Two crackers? A protein bar? The ambiguity is dangerous. We need standardized, quantified meal templates-not vague advice.
Christine Eslinger
November 19, 2025 AT 20:07I’m a pharmacist and I see this every single day. People think ‘take with food’ means ‘whenever you feel like eating.’ It doesn’t. It means ‘within 30 minutes of starting your meal.’
I had a 72-year-old patient taking glipizide on an empty stomach because she ‘didn’t eat breakfast.’ She passed out at the grocery store. We set a phone alarm for 30 mins before her 8am oatmeal. She’s been fine for 18 months now.
It’s not complicated. It’s just not taught well. Please, if you’re on more than three meds, sit down with your pharmacist. Not your doctor. Your pharmacist. They’re the real experts here.
Denny Sucipto
November 21, 2025 AT 08:36Bro, I took doxycycline with my Greek yogurt for three weeks and my UTI came back worse. Felt like my insides were being eaten by ants.
Then I remembered some Reddit post from 2020 said ‘don’t mix dairy with antibiotics.’ I waited two hours after yogurt. Took my pill. Didn’t touch dairy till dinner. Boom. Gone in 48 hours.
Don’t overthink it. Just don’t mix calcium with tetracycline. Simple.
Riohlo (Or Rio) Marie
November 22, 2025 AT 20:09Oh, so now we’re treating patients like lab rats with precisely timed gastric emptying windows? How quaint. The entire medical-industrial complex reduces human complexity to pharmacokinetic curves while ignoring the lived reality of people who work two jobs, have dementia, or live in food deserts.
‘Take levothyroxine 60 minutes before breakfast’-sure, if your breakfast is at 7 a.m. and you don’t have to drop your kid at daycare at 6:45. Or if you’re not a single parent who survives on coffee and a granola bar at 11 a.m.
Stop blaming patients. Fix the system. Or at least offer alternatives that don’t assume everyone lives in a 1950s nuclear family with a home-cooked meal at 8 a.m.
Leilani O'Neill
November 24, 2025 AT 07:54Irish people don’t even eat proper breakfasts anymore. Just a cuppa tea and a biscuit. No wonder our healthcare system is collapsing. You can’t expect a drug designed for a full American breakfast to work with a slice of brown bread and marmalade.
Stop Americanizing our medicine. We need Irish guidelines. No cola with itraconazole here-we drink tea. Tea doesn’t interfere. It’s natural. The FDA doesn’t understand our culture.
Shilpi Tiwari
November 26, 2025 AT 03:19From a pharmacokinetics perspective, the CYP3A4 inhibition by grapefruit juice is well-documented, but the real issue lies in inter-individual variability in CYP3A4 expression-particularly in South Asian populations where polymorphisms are more prevalent. The FDA’s food-effect models are largely Eurocentric and fail to account for dietary phytochemicals like curcumin and quercetin, which modulate intestinal permeability.
Moreover, the 2024 Nature Medicine circadian study overlooked chronotype-dependent gastric motility, which varies significantly between morning larks and night owls. A one-size-fits-all timing protocol is pharmacologically indefensible.
Louie Amour
November 26, 2025 AT 06:15I’ve been taking my Ozempic with breakfast for 8 months. Lost 40 lbs. Why? Because I didn’t read the label. The doctor didn’t tell me. My pharmacist? Never asked.
Now I’m reading this and realizing I’ve been doing it wrong. But I’m still losing weight. So what’s the point of all this science if it doesn’t change outcomes?
Maybe the real problem isn’t food-it’s that doctors don’t care enough to explain it.
Heidi R
November 27, 2025 AT 22:43You’re all missing the point. This isn’t about food. It’s about control. The medical system wants you to believe your body is too fragile to handle your own choices. So they give you rules. ‘Don’t eat with this.’ ‘Wait 30 minutes.’ ‘Only water.’
But your body knows what it needs. Trust yourself. I take my meds however I feel. I’m alive. I’m healthy. Your rules are just fear dressed up as science.
Hal Nicholas
November 29, 2025 AT 21:37They say ‘don’t take levothyroxine with coffee.’ But what if you’re a coffee addict? What if your entire identity is built around that first cup? You’re telling me I have to choose between my thyroid and my soul?
I don’t care about absorption percentages. I care about not crying at 3 p.m. because I’m exhausted. If I have to drink coffee 45 minutes after my pill, then so be it. I’ll live with the 10% loss. My mental health is more important than your bioavailability charts.
Conor McNamara
November 30, 2025 AT 13:22did you knwo that the fda and big pharma are in cahoots to make sure you keep taking meds? they dont want you to know that eating raw garlic every day cures everything. i took my doxycycline with garlic and it worked better. they buried the study. its on the dark web. check #medicationsarealies. they even made up the whole ‘food affects absorption’ thing to sell more pills.
Emanuel Jalba
December 1, 2025 AT 06:03THIS IS WHY WE CAN’T HAVE NICE THINGS 😭
I took my glipizide after lunch because I forgot. Had a panic attack, shaky hands, sweating like I was in a sauna. My wife called 911. I was 20 minutes from passing out.
Now I have a sticker on my pill bottle: ‘EAT BEFORE, NOT AFTER.’
My life is a minefield. I’m 32 and I have to treat my meds like a NASA launch. Someone please give me a goddamn app that texts me when to eat and when to not eat. I’m begging you.
Kristi Joy
December 2, 2025 AT 04:34Hey, if you’re reading this and you’re overwhelmed-breathe. You’re not failing. This stuff is confusing even for doctors. Start small: pick one med. Ask your pharmacist one question. Set one alarm. That’s enough.
You don’t have to be perfect. You just have to try. And if you mess up? It’s okay. Reset. Try again tomorrow. You’re doing better than you think.
And if you’re a caregiver? Be kind. This isn’t about blame. It’s about support.