The Science Behind Inflammation: Essential Facts You Must Know
 Oct, 17 2025
Oct, 17 2025
Inflammation Risk Assessment Tool
Assess your daily habits to understand your potential inflammation risk level. This tool is based on the scientific principles discussed in the article.
Your Inflammation Risk Assessment
Quick Takeaways
- Inflammation is the body’s natural alarm system, but chronic inflammation can fuel disease.
- Cytokines and prostaglandins are the chemical messengers that kick the response into gear.
- Acute inflammation heals; chronic inflammation harms organs over time.
- Diet, exercise, stress management, and proper sleep are the most effective daily tools.
- Seek medical advice when pain persists, swelling worsens, or you notice unexplained fatigue.
What Exactly Is Inflammation?
When your body spots a threat - a cut, a bug, or a chemical irritant - it lights up a cascade of signals to protect you. In plain terms, Inflammation is a complex biological response of the immune system aimed at eliminating the cause of cell injury, clearing out damaged tissue, and starting the healing process. Think of it as the emergency services rushing to a crash site: you get noise, traffic, and a lot of activity, but the goal is to get everyone safe again.
Key Players: The Chemical Messengers
The whole operation runs on tiny proteins and lipids that act like text messages.
- Cytokines are short‑range signaling proteins that tell immune cells where to go and what to do. Common examples include interleukin‑1 (IL‑1) and tumor necrosis factor‑alpha (TNF‑α). High levels of these molecules are a red flag for chronic inflammation.
- Prostaglandins are lipid compounds that cause blood vessels to expand, bring more blood to the site, and create the characteristic redness and heat. They also sensitize nerves, which is why inflamed areas often hurt.
These messengers don’t work alone - they recruit cells like Macrophages, the "big eaters" that gobble up debris and dead cells, and they trigger the release of enzymes that break down damaged tissue so it can be rebuilt.
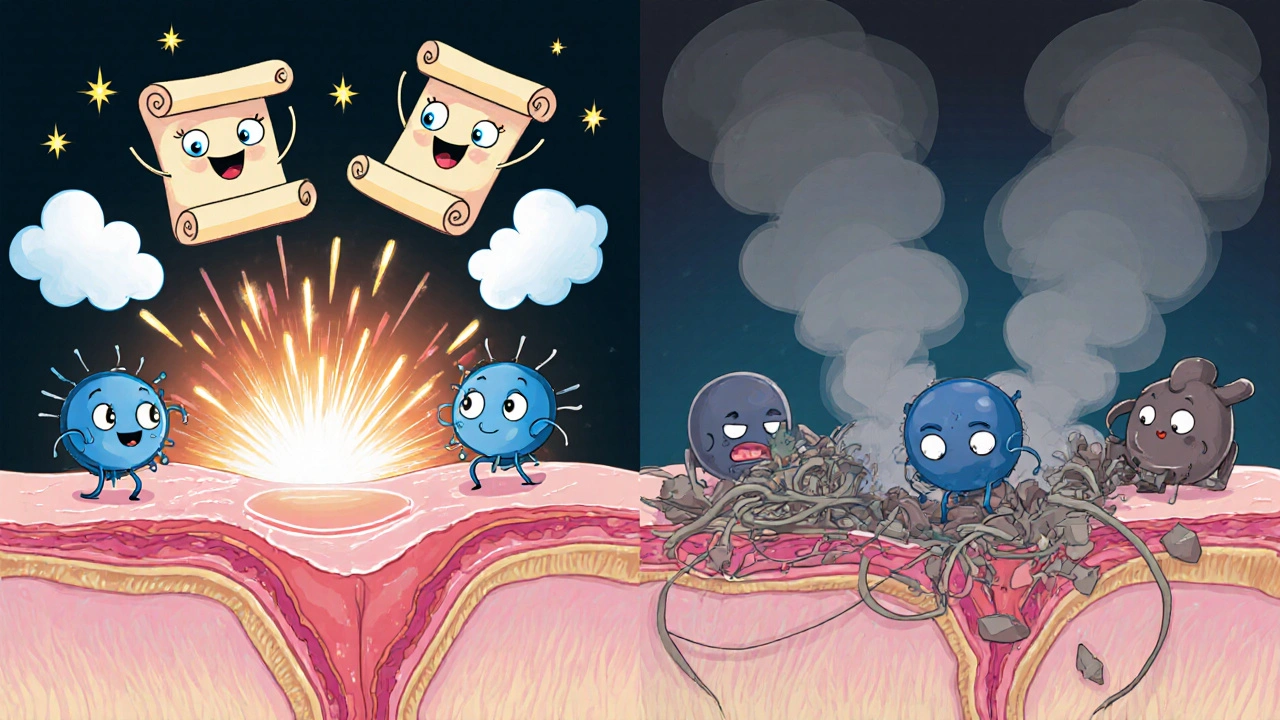
Acute vs. Chronic Inflammation
Not all inflammation is bad. The difference lies in duration and impact.
| Feature | Acute Inflammation | Chronic Inflammation |
|---|---|---|
| Typical duration | Minutes to a few weeks | Months to years |
| Primary purpose | Repair and eliminate immediate threat | Persistent low‑level immune activation |
| Common signs | Redness, heat, swelling, pain, loss of function | Fatigue, joint pain, low‑grade fever, tissue damage |
| Key cells involved | Neutrophils, macrophages | Macrophages, lymphocytes, fibroblasts |
| Associated diseases | Skin cuts, bacterial infections | Heart disease, type‑2 diabetes, rheumatoid arthritis, Alzheimer’s |
When acute inflammation clears a wound, the body returns to normal. When the response never fully shuts off, the lingering fire begins to scar organs - that’s chronic inflammation, the hidden driver behind many modern ailments.
Triggers of Chronic Inflammation
Multiple factors can keep the immune system in overdrive.
- Persistent infections (e.g., hepatitis C, periodontal disease)
- Excessive visceral fat - adipose tissue releases its own cytokines, known as adipokines.
- Environmental pollutants such as fine particulate matter (PM2.5) and cigarette smoke.
- Autoimmune misfires where the body attacks itself - rheumatoid arthritis is a classic example.
- Gut dysbiosis - an imbalanced Gut microbiome can leak bacterial fragments into the bloodstream, sparking systemic inflammation.
Managing Inflammation with Lifestyle Choices
The good news? You have a lot of control over the inflammation dial.
Dietary Strategies
Foods rich in Omega‑3 fatty acids (like salmon, mackerel, flaxseeds, and walnuts) compete with omega‑6 fats to produce less inflammatory prostaglandins. Aim for at least two servings of fatty fish per week.
Other anti‑inflammatory heroes include:
- Berries - packed with anthocyanins that neutralize oxidative stress.
- Leafy greens - source of vitamin K and polyphenols.
- Turmeric - contains curcumin, a potent inhibitor of NF‑κB, a key inflammation pathway.
Conversely, cut back on processed sugars, refined carbs, and excess red meat, all of which boost cytokine production.
Physical Activity
Moderate aerobic exercise (30 minutes, 5 days a week) lowers circulating IL‑6 and TNF‑α levels while increasing anti‑inflammatory IL‑10. Even brisk walking can shift the balance toward healing.
Stress Management
Chronic stress releases cortisol, which paradoxically can become dysregulated and raise inflammation over time. Mindfulness, deep‑breathing, or yoga can re‑tame the stress‑inflammation loop.
Sleep
Sleep deprivation spikes inflammatory markers. Aim for 7‑9 hours of consistent, restorative sleep; consider a dark, cool bedroom to maximize melatonin production.
When to Use Medications
Non‑steroidal anti‑inflammatory drugs (NSAIDs) such as ibuprofen block prostaglandin synthesis and provide quick relief for acute flare‑ups. They are not a long‑term fix for chronic inflammation because they can irritate the stomach lining and affect kidney function when used continuously.
For persistent inflammation, doctors may prescribe disease‑modifying agents (e.g., methotrexate for rheumatoid arthritis) that target specific cytokine pathways.
What Conditions Are Linked to Chronic Inflammation?
Understanding the connection helps you see why lifestyle tweaks matter.
- Cardiovascular disease: Inflammatory plaques in arteries can rupture, causing heart attacks.
- Type‑2 diabetes: Cytokine‑induced insulin resistance impairs glucose uptake.
- Alzheimer’s disease: Microglial activation and chronic brain inflammation accelerate plaque buildup.
- Rheumatoid arthritis: Autoimmune inflammation attacks joint linings, leading to deformities.
- Certain cancers: Inflammation can promote DNA damage and tumor growth.
When to Seek Professional Help
Most mild inflammation resolves on its own, but watch for these red flags:
- Swelling or pain that lasts more than two weeks without improvement.
- Fever above 100.4°F (38°C) that persists.
- Unexplained weight loss, night sweats, or chronic fatigue.
- Joint stiffness that’s worst in the morning and lasts over an hour.
These symptoms may signal an underlying autoimmune disorder or infection that needs targeted therapy.
Putting It All Together: A Practical Checklist
- Identify any persistent sore spots, joint pain, or unusual fatigue.
- Track diet for at least a week - note processed foods, sugar, and omega‑3 intake.
- Log weekly exercise minutes and sleep duration.
- Try a 10‑minute mindfulness routine each morning.
- If symptoms linger beyond two weeks, book a primary‑care appointment and discuss possible blood tests for CRP (C‑reactive protein) and ESR (erythrocyte sedimentation rate).
By following this simple loop, you can lower the chronic inflammation burden and protect long‑term health.
FAQ
What is the difference between acute and chronic inflammation?
Acute inflammation is a short‑term response that helps heal injuries and fight infections, lasting minutes to weeks. Chronic inflammation persists for months or years, often without a clear external threat, and can damage tissues and lead to disease.
Can diet really influence inflammation?
Yes. Foods high in omega‑3 fatty acids, antioxidants, and fiber help lower cytokine production, while excess sugar, refined carbs, and saturated fats boost inflammatory pathways. A balanced anti‑inflammatory diet can reduce markers like CRP.
Are NSAIDs safe for everyday use?
NSAIDs are fine for short‑term relief of pain or acute flare‑ups. Long‑term daily use can irritate the stomach lining, raise blood pressure, and affect kidney function, so they’re not recommended for chronic inflammation management without medical supervision.
How does stress cause inflammation?
Chronic stress triggers the release of cortisol and adrenaline. When these hormones stay elevated, they disrupt the normal feedback loop, leading to increased production of pro‑inflammatory cytokines like IL‑6 and TNF‑α.
What blood tests reveal inflammation?
Common markers include C‑reactive protein (CRP) and erythrocyte sedimentation rate (ESR). Elevated levels suggest systemic inflammation but don’t pinpoint the cause, so doctors combine them with clinical evaluation.
Understanding the science behind inflammation empowers you to spot trouble early and make everyday choices that keep the fire under control. inflammation isn’t just a medical term - it’s a signal that your body needs attention.

Emily Rankin
October 17, 2025 AT 16:06Imagine the body as a grand theater, its curtains rising whenever a wound or a rogue germ appears.
Inflammation is the spotlight that floods the stage, demanding every actor to play its part.
In that blazing moment, blood rushes like an eager audience, delivering oxygen and immune cells.
Cytokines whisper secret messages, telling the troops where to gather and what to demolish.
Prostaglandins fan the flames, making the scarlet hue and the throbbing ache that remind us we are alive.
When the curtain falls promptly, the scene resolves and the audience departs, leaving the body healed.
But when the lights never dim, the performance becomes a tragedy, etching scars into our organs.
Chronic inflammation is the endless encore that fuels heart disease, diabetes, and even the fog of dementia.
Yet hope glimmers in the choices we make each sunrise, for lifestyle is the master director of this drama.
A handful of wild salmon, rich in omega‑3, can coax the messengers to whisper softer, gentler notes.
Berries burst with antioxidants that mop up the rogue radicals lurking in the shadows.
A brisk walk in the morning is like a rehearsal that teaches the immune cast to stay disciplined.
When stress tries to hijack the script, a few minutes of mindful breathing can hand the pen back to calm.
Sleep, that quiet intermission, restores the stage and silences the inflammatory chorus.
Even if a flare-up threatens to steal the show, a short course of ibuprofen is the modest understudy that steadies the plot.
But we must remember that no pill can replace the steady rhythm of balanced meals and steady motion.
So let us cherish each day as an opportunity to turn down the volume of that fiery orchestra.
In doing so, we not only protect our own vessels but also set the stage for a brighter, healthier tomorrow.
Rebecca Mitchell
October 29, 2025 AT 04:52I was dealing with a swollen knee last week and I started adding turmeric to my coffee it actually helped the ache enough to jog again. Felt the relief instantly.
Roberta Makaravage
November 9, 2025 AT 18:39The molecular cascade you outlined is merely the tip of the iceberg that most people ignore 🙄. Cytokine storms don’t just happen in labs, they’re happening inside our bodies every time we overindulge in processed junk 😏. If you think a sprinkle of basil can magically mute IL‑6, you’re living in a fantasy world 🌱. The truth is, only a consistent anti‑inflammatory diet paired with regular aerobic exercise can sustainably lower CRP levels 👍. And let’s be clear, popping NSAIDs every day is like trying to put out a forest fire with a garden hose-ineffective and potentially harmful 🚒.
Lauren Sproule
November 21, 2025 AT 08:26Hey Roberta, i get what you’re saying but lets not forget balance is key so while omega‑3 is great remember that even a small treat now and then isn’t the end of the world. Also dont discount the power of simple habits like walking or drinking enough water they definatly help keep the inflammation in check. And hey, we all slip up sometimes, it’s all about getting back on track together 🙂.
CHIRAG AGARWAL
December 2, 2025 AT 22:12Honestly this whole rundown feels way too long for what could have been a quick tip list. I mean, who has time to read all that when you’re just trying to figure out why your back hurts? Some of those details could have been summed up in a single paragraph.
Carissa Padilha
December 14, 2025 AT 11:59It’s not just about length, it’s about the hidden agenda that stalls us from seeing the real culprits. The pharma giants deliberately flood the internet with endless scientific jargon to keep us confused and buying their overpriced drugs. While we’re busy counting cytokine names, they’re polishing the next big prescription that will lock us in a cycle of dependency. The truth is the “lifestyle fixes” they mention are just a distraction from the fact that the system is rigged against anyone who tries to go natural. So read between the lines and don’t let the noise drown out the reality.
Richard O'Callaghan
December 26, 2025 AT 01:46I think the post covered a lot but some points were a bit overcomplicated for the average reader. For exampel, the part about NF‑kB could have been explained wih a simple analogy. Also, a few typos slipped in like “prosta glandins” instead of prostaglandins which might confuse newbies.
Alexis Howard
January 6, 2026 AT 15:32Inflammation is a myth.