Thyroid Ultrasound: How Imaging Nodules Helps Assess Cancer Risk
 Feb, 1 2026
Feb, 1 2026
Most people never know they have a thyroid nodule until it shows up on an ultrasound. These small lumps in the thyroid gland are incredibly common - found in up to 68% of adults during routine imaging. But here’s the thing: thyroid ultrasound isn’t just about finding nodules. It’s about figuring out which ones need attention and which ones can be safely ignored.
Why Ultrasound Is the First Step
If your doctor finds a lump in your neck or your blood tests show something off, the next step isn’t a biopsy. It’s an ultrasound. That’s because ultrasound is the only imaging tool that gives real-time, detailed pictures of the thyroid without radiation, needles, or contrast dye. It’s fast, cheap (usually $200-$500 in the U.S.), and safe enough to repeat if needed. Unlike CT or MRI scans, which mostly spot nodules by accident, ultrasound is built for this job. It can see nodules as small as 2-3 millimeters - way smaller than what you’d feel with your fingers. In fact, physical exams miss more than half of all nodules. Ultrasound catches them all.What Doctors Look For: The Five Key Signs
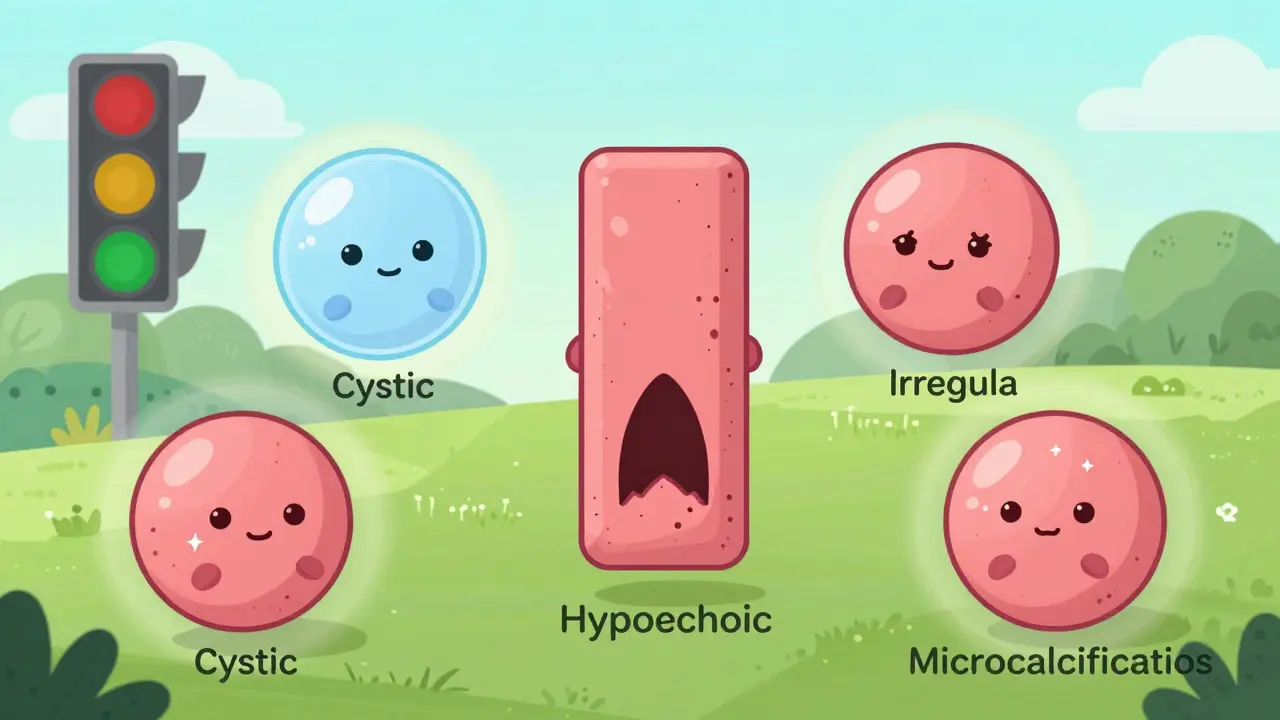
Not all nodules are the same. Some are harmless fluid-filled sacs. Others look suspicious because of how they’re shaped, how they reflect sound, or how blood flows through them. Radiologists check five main features:- Composition: Is it mostly fluid (cystic), full of spongy tissue (spongiform), mixed, or solid? Solid nodules carry more risk.
- Echogenicity: How bright or dark does it look compared to the surrounding thyroid tissue? Markedly hypoechoic (very dark) nodules are more likely to be cancerous.
- Shape: Is it taller than it is wide? That’s a red flag. Normal nodules are wider than they are tall.
- Margin: Smooth edges? Usually fine. Jagged, irregular, or spreading beyond the thyroid? That’s concerning.
- Punctate echogenic foci: Tiny white dots inside the nodule - called microcalcifications - are one of the strongest predictors of cancer.
These features are scored using something called TI-RADS - the Thyroid Imaging Reporting and Data System. It’s like a traffic light for nodules:
- TR1 (0 points): 0.3% chance of cancer - no follow-up needed.
- TR2 (2 points): 1.5% risk - monitor if large.
- TR3 (3 points): 4.8% risk - consider biopsy if over 2.5 cm.
- TR4 (4-6 points): 9.1% risk - biopsy recommended.
- TR5 (7+ points): 35% risk - high chance of cancer, biopsy is urgent.
This system replaced older, less reliable guidelines. Studies show TI-RADS predicts cancer risk far better than just guessing based on size alone.
When Biopsy Is Necessary - And When It’s Not
Ultrasound tells you the risk. But it can’t confirm cancer. Only a biopsy can do that. Still, not every suspicious nodule needs a needle.If a nodule is under 5 mm - even if it looks risky - most doctors won’t biopsy it. The chance it’s dangerous is so low, the risks of the procedure outweigh the benefits. Instead, they’ll just keep an eye on it.
For nodules 1 cm or larger with suspicious features (like microcalcifications or irregular margins), fine-needle aspiration (FNA) is standard. But here’s the twist: ultrasound doesn’t just guide the biopsy - it makes it better. When done with ultrasound guidance, the rate of unclear results drops from 25% to under 5%. That means fewer repeat procedures.
Even after a biopsy, things aren’t always clear. About 15-30% of results are indeterminate - meaning the cells look weird but not clearly cancerous. That’s where molecular testing comes in. New gene tests can now tell you whether an indeterminate nodule is likely benign, cutting unnecessary surgeries by about half. But even then, you still need follow-up ultrasounds. Cancer can grow slowly. You can’t just walk away after one test.
What Ultrasound Can’t Do
Ultrasound is powerful, but it’s not magic. It can’t see nodules that have grown far down into the chest (substernal goiters). It can’t tell you for sure if a nodule is cancerous - only how likely it is. And it can’t replace the biopsy.Some people think a thyroid scan (using radioactive iodine) is better. But those scans only show if a nodule is "hot" (overactive) or "cold" (underactive). Hot nodules almost never turn cancerous. Cold ones have about a 15% risk - but the scan doesn’t tell you which cold nodules are dangerous. That’s why ultrasound is always the first step. Scans are only used in rare cases, like when someone has abnormal thyroid hormone levels.
CT and MRI scans? They’re great for big tumors or when cancer has spread. But they can’t see the fine details - like microcalcifications or shape - that tell you if a nodule is risky. They’re not used for initial screening.
The Rise of AI and Better Tools
New tech is changing how ultrasounds are read. A 2023 study in Nature Scientific Reports showed a new AI model could analyze nodules with 94.2% accuracy - higher than even experienced radiologists. It looked at shape, texture, and how the nodule sits in the gland, using attention algorithms to focus on the most telling signs.This isn’t science fiction. AI tools are already being tested in clinics. They help reduce human error - especially in places where experts are scarce. Inter-observer variability (when two doctors disagree on the same image) is still a problem. Studies show agreement on margin assessment is only around 50-65%. AI can help fix that.
Another advance is elastography - measuring how stiff a nodule is. Cancerous tissue tends to be harder than healthy tissue. And contrast-enhanced ultrasound, which uses tiny bubbles to track blood flow, gives more detail on vascularity. But these are still extras. The core remains grayscale and Doppler ultrasound.

What Happens After the Scan?
If your nodule is low risk (TR1 or TR2), you might never see a doctor about it again. No treatment. No surgery. Just peace of mind.If it’s medium risk (TR3), you’ll likely get a follow-up ultrasound in 1-2 years. If it doesn’t grow, you’re probably fine.
If it’s high risk (TR4 or TR5), you’ll get a biopsy. If cancer is confirmed, treatment depends on size, type, and your age. Many small papillary cancers (under 1 cm) are now managed with active surveillance - meaning you get regular ultrasounds instead of immediate surgery. The 10-year survival rate? Over 99%. Surgery isn’t always the answer.
And if your biopsy is indeterminate? Molecular testing helps. But you still need ultrasound checks every 6-12 months. Even if the gene test says "benign," you can’t ignore the nodule. It might change later.
Who Should Get One?
The guidelines are clear: if you have a thyroid nodule - whether you felt it or not - you should get an ultrasound. That includes people with:- A lump or swelling in the neck
- Abnormal thyroid blood tests (TSH, T3, T4)
- A history of radiation to the head or neck
- A family history of thyroid cancer
- Incidental findings on other scans (like a CT for a head injury)
Even if you feel fine, if your doctor sees a nodule on a scan, they should order an ultrasound. It’s the only way to know what you’re dealing with.
What About the Future?
The next big step? Combining ultrasound features with molecular data. Imagine a report that says: "This nodule has a 7% cancer risk based on shape and calcifications - and your gene profile shows no mutations linked to aggressive cancer. Watch for now." That’s what experts are working toward. By 2030, personalized risk scores could cut unnecessary biopsies by 30%.For now, ultrasound remains the gold standard. It’s safe, accurate, and widely available. No other tool comes close. And with AI improving its precision, it’s only getting better.

Ellie Norris
February 2, 2026 AT 11:47so i had a nodule last year and my doc just said "eh, probably fine" and sent me on my way. turns out it was TR3 and i didn’t even know until i checked my old records. glad i found this post - learned way more than my endocrinologist told me 😅
Marc Durocher
February 2, 2026 AT 14:03so like… if you’re gonna get an ultrasound, why not just skip to the biopsy? i mean, we all know the system’s broken. but hey, at least the ultrasound doesn’t cost a kidney. or a mortgage. or my dignity.
larry keenan
February 3, 2026 AT 18:58The diagnostic utility of grayscale and Doppler ultrasonography in thyroid nodule evaluation remains the cornerstone of clinical assessment due to its high spatial resolution, lack of ionizing radiation, and reproducibility across diverse healthcare settings. The TI-RADS classification system, while not universally adopted, demonstrates improved interobserver reliability compared to prior lexicons and enables risk-stratified management protocols. Further integration of elastographic and contrast-enhanced modalities may augment predictive accuracy, though standardization remains a challenge in community practice.
Nick Flake
February 5, 2026 AT 07:09imagine if your body was a Netflix show and your thyroid was the main character 🤔
some nodules? just background extras. chill, no plot twist.
others? full villain arc with microcalcifications as the ominous red lighting and jagged margins like the villain’s laugh. 😱
and ai? the genius sidekick who sees the pattern before anyone else.
we’re not just scanning tissue - we’re reading destiny. and somehow, it’s still cheaper than a gym membership.
Akhona Myeki
February 7, 2026 AT 06:26In South Africa, we do not waste resources on unnecessary ultrasounds. If a man has a lump, he goes to the clinic and gets a proper diagnosis - not some American overtesting ritual. We respect the body. We do not panic at every speck. Your system is bloated. We manage with less and achieve better outcomes.
Chinmoy Kumar
February 7, 2026 AT 13:12hey i just found out my mom had a nodule last year and they watched it for 18 months and it never changed. i never knew thyroid stuff could be so chill. like, we dont need to fix everything right away. sometimes just watching is the bravest thing you can do 🙏
Brett MacDonald
February 8, 2026 AT 22:57so like… if ai can read ultrasounds better than docs, why do we even have docs? are we just decoration now? i mean, i’m not mad, just curious. also, my phone can probably do this now. i think i’ll just take a pic of my neck and send it to chatgpt
Sandeep Kumar
February 10, 2026 AT 09:52why do americans need 5 different tests for a lump? in India we have one doctor one glance and he knows. no fancy machines no ai no ti-rads. just experience. you think your tech is better? you just scared of trusting people
Gary Mitts
February 11, 2026 AT 20:03biopsy? nah. just wait. it’ll either grow or vanish. either way, you’re not dying. chill.
Dan Pearson
February 13, 2026 AT 17:39oh so now we’re using AI to diagnose thyroid nodules? wow. next they’ll use a TikTok filter to detect cancer. meanwhile, real doctors are getting paid less while algorithms get promoted. this is the future? i’d rather get poked with a needle than trust a robot that doesn’t even know what coffee tastes like.
Eli Kiseop
February 15, 2026 AT 07:49so if my nodule is TR1… does that mean i can stop Googling it? because i’ve been down the rabbit hole for 3 weeks now and i’m convinced i have stage 4 medullary cancer even though i’ve never had a single symptom