HIV Medications with Statins: Safe Choices and Side Effects
 Jan, 10 2026
Jan, 10 2026
HIV Statin Interaction Checker
This tool helps you determine if your HIV medications interact dangerously with statins. It identifies safe statin choices and dose adjustments based on your specific regimen.
People living with HIV are living longer than ever before. But with that longevity comes a new challenge: managing heart disease risk. Statins, the go-to drugs for lowering cholesterol, are often needed. But mixing them with HIV medications? That’s where things get risky. Not all statins are safe. Some can cause dangerous muscle damage-even life-threatening rhabdomyolysis-if taken with certain HIV drugs. The key isn’t avoiding statins altogether. It’s knowing which ones you can use, and how to use them safely.
Why HIV Drugs and Statins Don’t Always Mix
Most HIV medications are processed by the liver using enzymes called CYP3A4 and transporters like OATP1B1. So are many statins. When both are taken together, one drug can block the other’s breakdown. That means the statin builds up in your blood-sometimes to levels 20 times higher than normal. That’s not just a minor bump. It’s a red flag for muscle pain, weakness, and kidney damage. The worst offenders are the boosted HIV drugs: those with cobicistat or ritonavir. These aren’t the main HIV fighters themselves-they’re boosters. They make other HIV drugs work better by slowing down how fast your body breaks them down. But they also slow down statin clearance. That’s why drugs like darunavir/cobicistat (Symtuza, Prezcobix) and atazanavir/ritonavir (Reyataz) are the biggest red flags.Statins You Must Avoid Completely
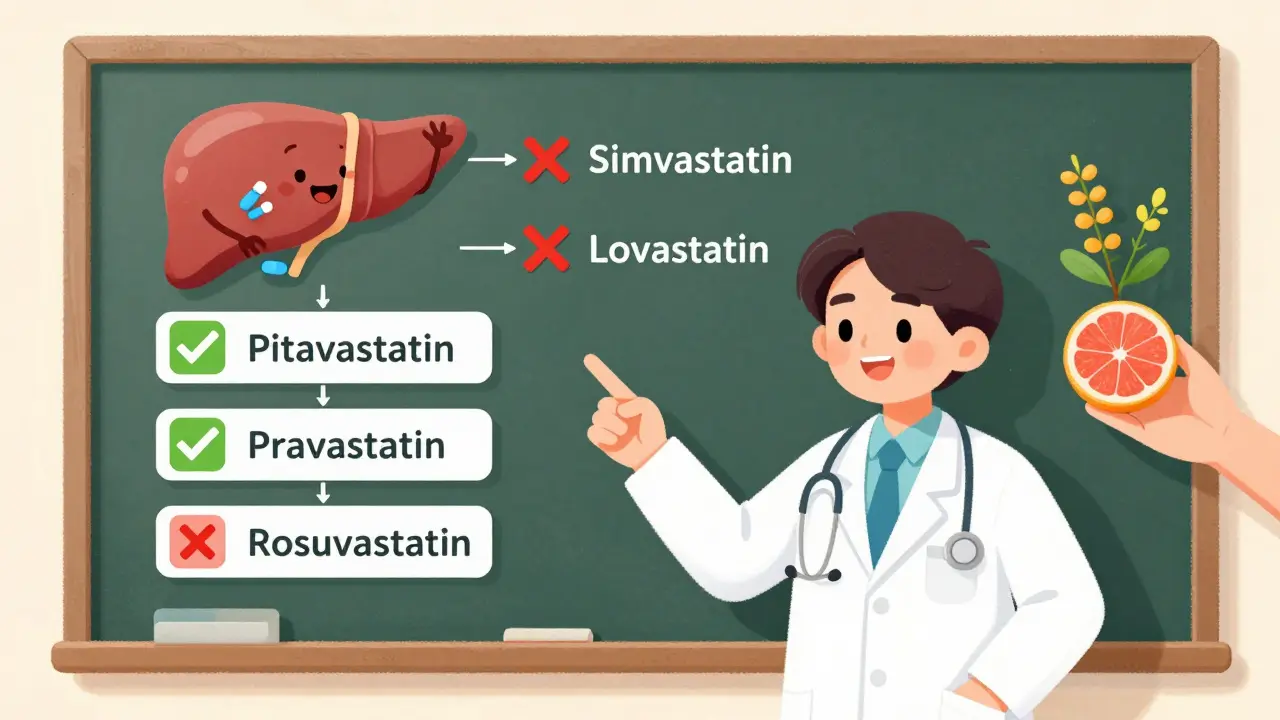
If you’re on any boosted HIV regimen, there are two statins you should never take: simvastatin (Zocor) and lovastatin (Mevacor). This isn’t a "use with caution" warning. This is a hard no. The FDA and major HIV guidelines all agree: these two are contraindicated. Why? Because they’re almost entirely broken down by CYP3A4. When cobicistat or ritonavir blocks that pathway, simvastatin levels can spike by up to 20-fold. There have been real cases of people ending up in the hospital with muscle breakdown, kidney failure, and even death. No one should ever take simvastatin or lovastatin with darunavir, atazanavir, lopinavir, or any cobicistat-containing pill.Safe Statin Options and Their Limits
Good news: you have choices. Not all statins are created equal. Some use different liver pathways and play nicer with HIV drugs.- Pitavastatin (Livalo): This is the top pick. It barely touches CYP3A4. Most HIV regimens, even boosted ones, don’t affect it much. You can usually take the full dose-4 mg daily-without adjustment.
- Pravastatin (Pravachol): Also low risk. It doesn’t rely on CYP3A4. Safe with most HIV meds. Dose: 10-40 mg daily.
- Rosuvastatin (Crestor): Works well, but with limits. With ritonavir or cobicistat, your dose must stay at or below 10 mg daily. Higher doses can raise levels too much.
- Atorvastatin (Lipitor): The most common statin. Safe if you keep the dose low. With cobicistat, don’t go over 20 mg daily. With unboosted regimens, 40 mg is usually fine.
- Fluvastatin (Lescol): Less used, but an option. It’s broken down by CYP2C9, not CYP3A4. But if you’re on ritonavir, your dose may need to be cut in half.
What About Newer HIV Drugs?
The newer HIV medications-especially integrase inhibitors like dolutegravir (Tivicay), bictegravir (in Biktarvy), and raltegravir (Isentress)-are much safer with statins. They don’t strongly interfere with liver enzymes. That means if you’re on one of these, you can usually take standard doses of atorvastatin, rosuvastatin, or even pitavastatin without major adjustments. This is why doctors now prefer starting new patients on integrase-based regimens if they also need a statin. It simplifies treatment. Fewer interactions. Fewer pills to worry about. Fewer trips to the pharmacy to check for conflicts.Monitoring: What You Need to Watch For
Even with the safest choices, you still need to be watched. Muscle pain isn’t always obvious. It might start as mild soreness, like after a workout. But if it gets worse, or you notice dark urine, stop the statin and call your doctor right away. Your provider should check:- Creatine kinase (CK) levels-before starting and after 4-6 weeks
- Liver enzymes (ALT, AST)
- Kidney function (creatinine)
Other Medications to Watch Out For
It’s not just HIV drugs. Many other common meds can make statin risks worse:- Gemfibrozil (for high triglycerides): Never mix with statins. It increases muscle damage risk. Use fenofibrate instead.
- Calcium channel blockers: Felodipine, diltiazem, verapamil-all can interfere. Ask your doctor if you can switch to amlodipine or lisinopril.
- Antifungals: Fluconazole, itraconazole, ketoconazole-avoid with statins.
- Herbal supplements: St. John’s wort can lower statin levels, making them less effective. Grapefruit juice? Skip it. It boosts statin levels.
What You Should Do Right Now
If you’re on HIV meds and take a statin-or your doctor just suggested one-here’s what to do:- Check your current statin. Is it simvastatin or lovastatin? If yes, ask your doctor to switch you immediately.
- Know your HIV regimen. Are you on cobicistat or ritonavir? If yes, your statin dose may need to be lowered.
- Use a reliable drug interaction checker. The University of Liverpool’s HIV Drug Interactions website (hiv-druginteractions.org) is the gold standard. It’s updated monthly and used by clinics worldwide.
- Bring a full list of all your meds to every appointment-including vitamins, supplements, and over-the-counter painkillers.
- Report any new muscle pain, weakness, or dark urine right away. Don’t wait.
Why This Matters More Than Ever
Back in 2007, about 15% of people with HIV were on statins that were unsafe with their HIV drugs. By 2015, that number dropped to under 5%. That’s progress. But here’s the problem: only 40-60% of people who need a statin are getting one at all. Too many are still skipping them out of fear, or because their provider doesn’t know the right options. Heart disease is now the leading cause of death in people with HIV-not AIDS. Statins save lives. But only if they’re used correctly. The right statin, at the right dose, with the right HIV drug, can cut your risk of heart attack and stroke by half.Final Takeaway
You don’t have to choose between managing your HIV and protecting your heart. You can do both. But you need to be smart about it. Avoid simvastatin and lovastatin. Pick pitavastatin or pravastatin if you can. If you need rosuvastatin or atorvastatin, stick to the low doses. Always check for interactions. And never assume your doctor knows every possible conflict-ask them to use a trusted tool like the Liverpool database. Your heart matters. Your HIV treatment matters. And with the right choices, they don’t have to fight each other.Can I take atorvastatin with my HIV meds?
Yes, but only if your HIV regimen allows it. If you’re taking cobicistat (like in Symtuza or Prezcobix), limit atorvastatin to 20 mg daily. If you’re on an unboosted integrase inhibitor like dolutegravir or bictegravir, you can usually take up to 40 mg daily. Never take atorvastatin with ritonavir or cobicistat above 20 mg without close monitoring.
Is rosuvastatin safe with HIV drugs?
Rosuvastatin is safe with most HIV drugs, but your dose must be limited. With ritonavir or cobicistat, do not exceed 10 mg daily. With integrase inhibitors like dolutegravir, 10-20 mg is generally acceptable. Higher doses can raise blood levels too much and increase muscle damage risk.
Why can’t I take simvastatin with HIV meds?
Simvastatin is broken down almost entirely by the CYP3A4 enzyme. HIV boosters like cobicistat and ritonavir block this enzyme, causing simvastatin to build up in your blood-sometimes by 20 times. This dramatically increases the risk of rhabdomyolysis, a dangerous condition that breaks down muscle tissue and can lead to kidney failure or death.
What’s the safest statin for someone with HIV?
Pitavastatin is generally the safest. It doesn’t rely on CYP3A4, so most HIV drugs don’t interfere with it. Pravastatin is also very low risk. Both can usually be taken at full doses without adjustment, even with boosted HIV regimens. They’re the top choices for people who need both HIV treatment and a statin.
Should I get my muscle enzymes checked if I’m on a statin with HIV meds?
Yes. Your doctor should check your creatine kinase (CK) levels before you start the statin and again 4-6 weeks after starting or changing the dose. They should also monitor liver enzymes and kidney function. If you develop unexplained muscle pain, weakness, or dark urine, stop the statin and contact your provider immediately.
Can I take over-the-counter supplements with my statin and HIV meds?
Be very careful. St. John’s wort can lower statin levels, making them less effective. Grapefruit juice increases statin levels and can be dangerous with boosted HIV drugs. Omega-3 fatty acids and fenofibrate are safer for triglycerides than gemfibrozil. Always tell your doctor about every supplement you take-even if you think it’s harmless.
Do long-acting HIV injections affect statins?
Yes. Long-acting injectables like cabotegravir and rilpivirine stay in your body for months. Even after your last shot, they can still interact with statins. This means interaction risks don’t disappear after you stop taking pills. Always inform your provider if you switch to or from long-acting HIV treatments.
How do I know if my doctor is using the right resources?
Ask them. The University of Liverpool’s HIV Drug Interactions website (hiv-druginteractions.org) is the most trusted, up-to-date tool used by HIV specialists worldwide. If your doctor doesn’t use it or a similar validated resource before prescribing a statin, ask why. Many primary care providers still rely on memory or outdated guidelines, which can be dangerous.

Jennifer Phelps
January 11, 2026 AT 01:22Just started pitavastatin last month after my HIV doc flagged my old simvastatin as dangerous
Wish I’d known sooner-my legs were aching like I’d run a marathon every day
Now I feel fine and my cholesterol’s down
Why isn’t this info more common?
Rinky Tandon
January 11, 2026 AT 19:23Let me be crystal clear-this isn’t just about statins, it’s about systemic medical negligence
Doctors are still prescribing simvastatin to PLWH like it’s 2008
And patients? They’re dying quietly because no one bothered to check drug interactions
This is malpractice wrapped in apathy
And don’t even get me started on how pharma pushes dangerous combos because they’re profitable
Wake up people, this isn’t a suggestion-it’s a massacre waiting to happen
Ben Kono
January 12, 2026 AT 22:42My doc put me on atorvastatin 20mg with my boosted regimen
Didn’t even tell me why the dose was capped
Found out on my own by reading the Liverpool site
Why do docs assume we’ll just trust them without explaining the why
Cassie Widders
January 13, 2026 AT 08:56My doctor recommended pitavastatin too. It’s been smooth. No muscle pain, no weird side effects. Just quiet, steady progress. I’m glad I listened.
Konika Choudhury
January 14, 2026 AT 17:24Why do Americans always act like they invented medical knowledge
Indian doctors have been warning about statin-HIV combos since 2012
We had our own guidelines before you even knew what cobicistat was
Stop acting like this is new news
jordan shiyangeni
January 15, 2026 AT 20:33It’s not merely a pharmacokinetic issue-it’s a catastrophic failure of clinical diligence and institutional accountability
The fact that simvastatin was ever co-prescribed with ritonavir-boosted regimens constitutes a gross deviation from the standard of care
And yet, in 2024, primary care physicians continue to rely on outdated formularies, cognitive biases, and incomplete electronic health record alerts
This is not negligence-it’s systemic epistemic failure
Patients are being sacrificed on the altar of convenience and ignorance
And the worst part? The same clinicians who prescribe these dangerous combos are the ones who will feign surprise when the CK levels skyrocket and the patient is admitted to the ICU with rhabdomyolysis
There is no excuse. None.
Abner San Diego
January 17, 2026 AT 17:40Yeah but like… how many people actually die from this?
Seems like everyone’s freaking out over a few cases
My cousin’s on simvastatin with his HIV meds and he’s fine
Maybe we’re overreacting?
Eileen Reilly
January 17, 2026 AT 17:45lol i just took my statin with my HIV pill and didnt think twice
then i saw this post and panicked
but then i checked my med list and i’m on pitavastatin so im chill
but wow like… why is this so hard to find out
my doctor never mentioned any of this
and i’ve been on this combo for 3 years
thanks internet
steve ker
January 18, 2026 AT 18:15Pitavastatin is the only rational choice. Everything else is a gamble. The rest of this post is just noise.
Sonal Guha
January 20, 2026 AT 02:55My doctor told me to avoid grapefruit juice but never said why
Now I know
Also I take fenofibrate instead of gemfibrozil
Thanks for the checklist